
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Basic Research
- Carnitine Orotate Complex Ameliorates Insulin Resistance and Hepatic Steatosis Through Carnitine Acetyltransferase Pathway
- Jung-Hee Hong, Moon-Kyu Lee
- Diabetes Metab J. 2021;45(6):933-947. Published online August 19, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0223
- 5,785 View
- 167 Download
- 3 Web of Science
- 3 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 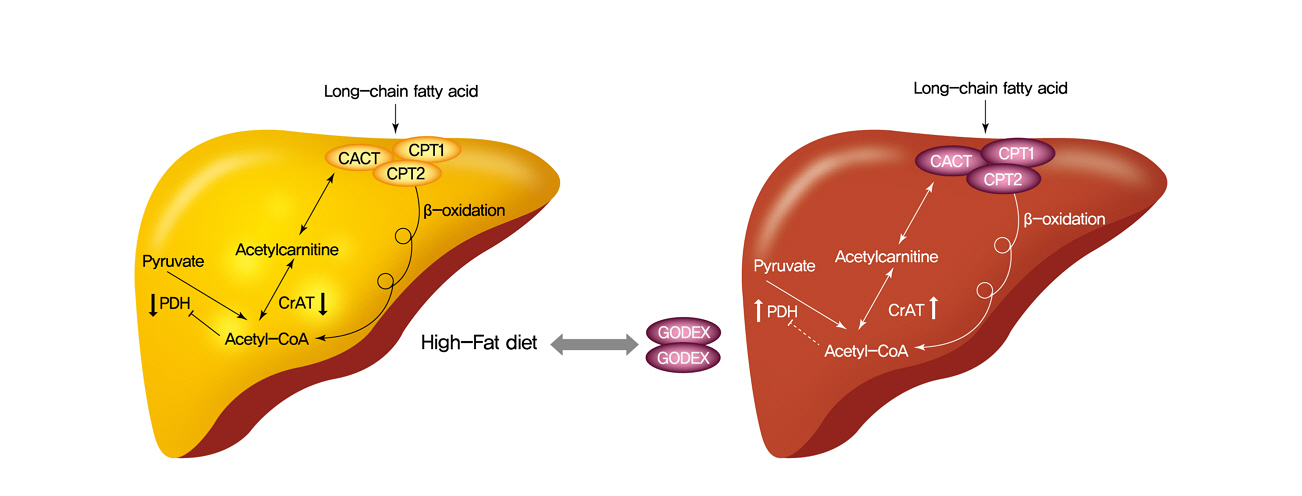
- Background
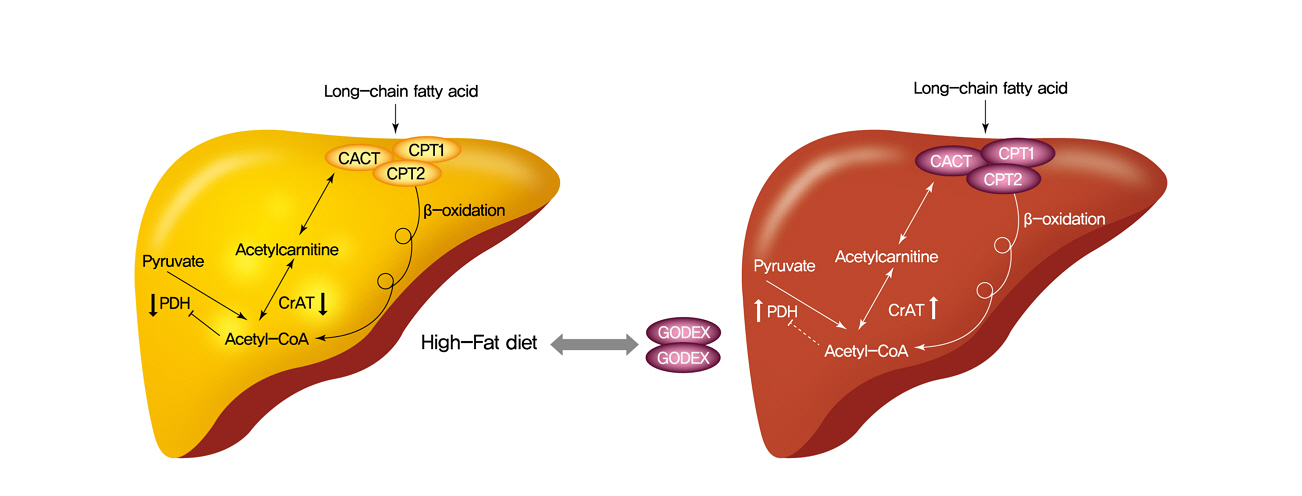
Carnitine orotate complex (Godex) has been shown to decrease glycated hemoglobin levels and improve steatosis in patients with type 2 diabetes mellitus with non-alcoholic fatty liver disease. However, the mechanisms of Godex in glucose metabolism remain unclear.
Methods
Male C57BL/6J mice were divided into four groups: normal-fat diet, high-fat diet, a high-fat diet supplemented with intraperitoneal injection of (500 mg or 2,000 mg/kg/day) Godex for 8 weeks. Computed tomography, indirect calorimetry, and histological analyses including electron microscopy of the liver were performed, and biochemical profiles and oral glucose tolerance test and insulin tolerance test were undertaken. Expressions of genes in the lipid and glucose metabolism, activities of oxidative phosphorylation enzymes, carnitine acetyltransferase, pyruvate dehydrogenase, and acetyl-coenzyme A (CoA)/CoA ratio were evaluated.
Results
Godex improved insulin sensitivity and significantly decreased fasting plasma glucose, homeostatic model assessment for insulin resistance, steatosis, and gluconeogenesis, with a marked increase in fatty acid oxidation as well as better use of glucose in high-fat diet-fed mice. It preserved mitochondrial function and ultrastructure, restored oxidative phosphorylation enzyme activities, decreased acetyl-CoA/CoA ratio, and increased carnitine acetyltransferase content and pyruvate dehydrogenase activity. Carnitine acetyltransferase knockdown partially reversed the effects of Godex in liver and in vitro.
Conclusion
Godex improved insulin resistance and steatosis by regulating carnitine acetyltransferase in liver in high-fat diet-fed mice. -
Citations
Citations to this article as recorded by- Impact of l-Carnitine Supplementation on Liver Enzyme Normalization in Patients with Chronic Liver Disease: A Meta-Analysis of Randomized Trials
Hyunwoo Oh, Chan Hyuk Park, Dae Won Jun
Journal of Personalized Medicine.2022; 12(7): 1053. CrossRef - Prolonged Use of Carnitine-Orotate Complex (Godex®) Is Associated with Improved Mortality: A Nationwide Cohort Study
Kye-Yeung Park, Sangmo Hong, Kyung-Soo Kim, Kyungdo Han, Cheol-Young Park
Journal of Personalized Medicine.2022; 12(12): 1970. CrossRef - The Role of Carnitine Orotate Complex in Fatty Liver
Hyon-Seung Yi
Diabetes & Metabolism Journal.2021; 45(6): 866. CrossRef
- Impact of l-Carnitine Supplementation on Liver Enzyme Normalization in Patients with Chronic Liver Disease: A Meta-Analysis of Randomized Trials
- Complications
- Association of Urinary N-Acetyl-β-D-Glucosaminidase with Cardiovascular Autonomic Neuropathy in Type 1 Diabetes Mellitus without Nephropathy
- Min Sun Choi, Ji Eun Jun, Sung Woon Park, Jee Hee Yoo, Jiyeon Ahn, Gyuri Kim, Sang-Man Jin, Kyu Yeon Hur, Moon-Kyu Lee, Jae Hyeon Kim
- Diabetes Metab J. 2021;45(3):349-357. Published online February 2, 2021
- DOI: https://doi.org/10.4093/dmj.2019.0211
- 5,631 View
- 121 Download
- 1 Web of Science
- 2 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 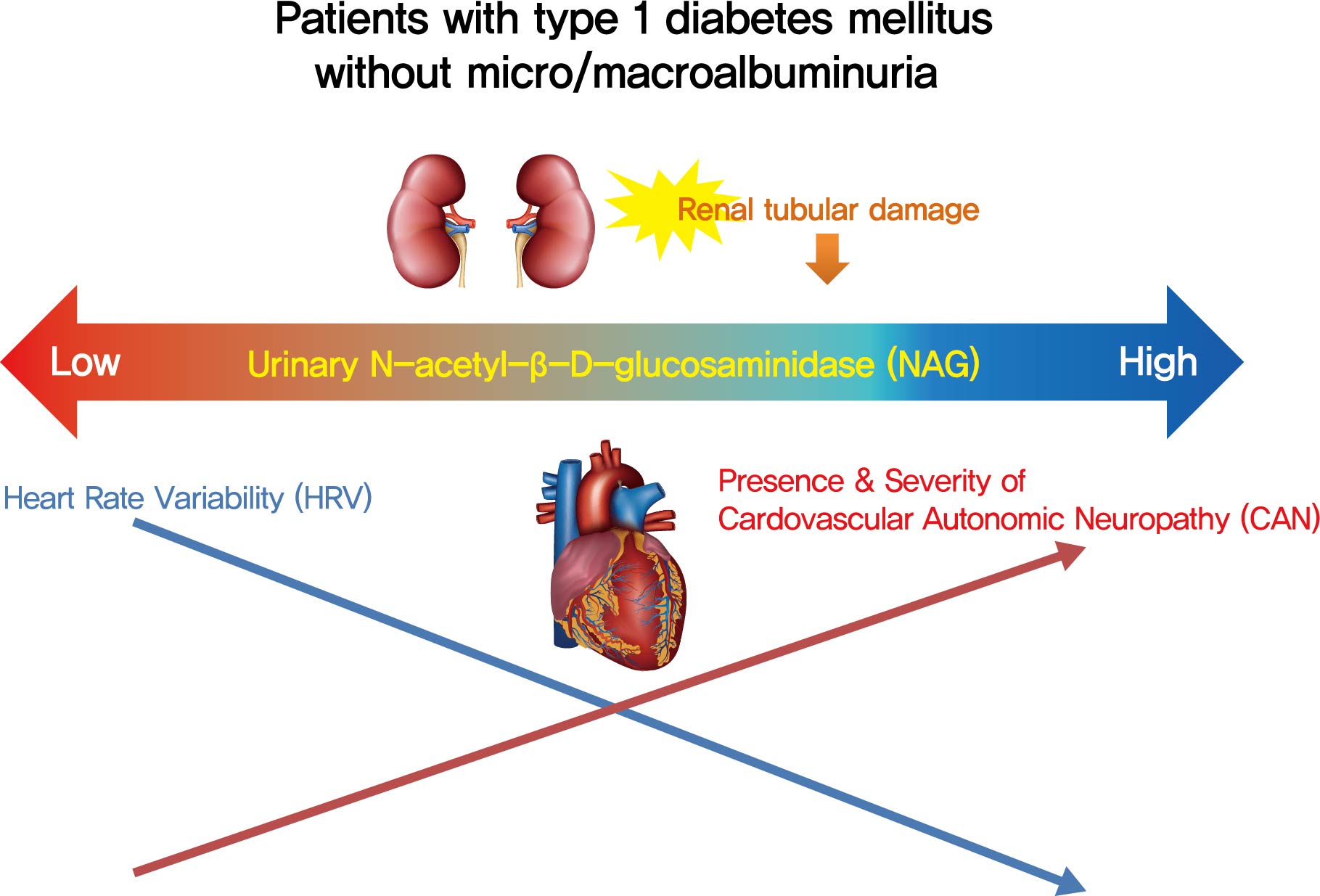
- Background
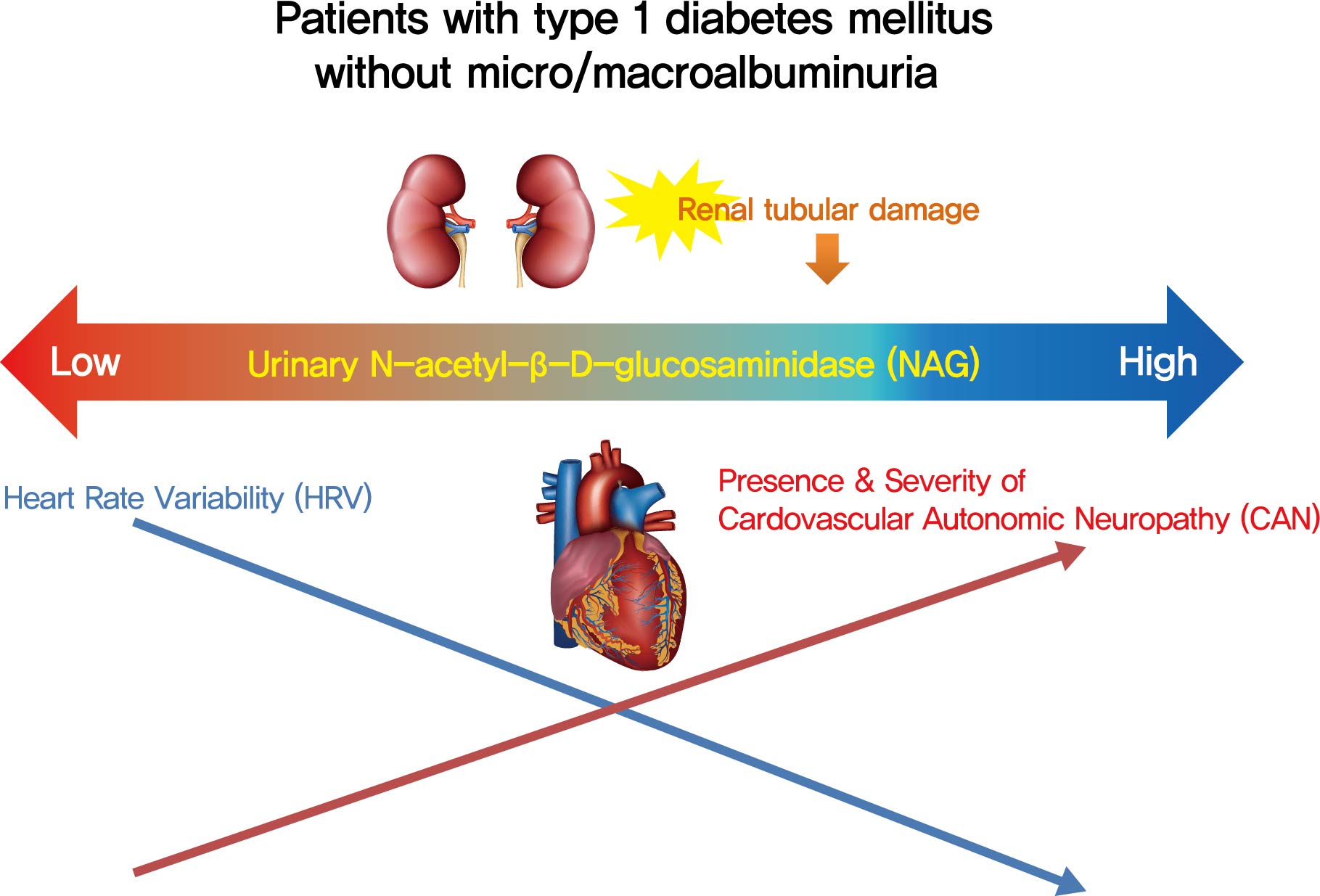
Cardiovascular autonomic neuropathy (CAN) is a common microvascular complication of diabetes and related to albuminuria in diabetic nephropathy (DN). Urinary N-acetyl-β-D-glucosaminidase (uNAG) is a renal tubular injury marker which has been reported as an early marker of DN even in patients with normoalbuminuria. This study evaluated whether uNAG is associated with the presence and severity of CAN in patients with type 1 diabetes mellitus (T1DM) without nephropathy.
Methods
This cross-sectional study comprised 247 subjects with T1DM without chronic kidney disease and albuminuria who had results for both uNAG and autonomic function tests within 3 months. The presence of CAN was assessed by age-dependent reference values for four autonomic function tests. Total CAN score was assessed as the sum of the partial points of five cardiovascular reflex tests and was used to estimatethe severity of CAN. The correlations between uNAG and heart rate variability (HRV) parameters were analyzed.
Results
The association between log-uNAG and presence of CAN was significant in a multivariate logistic regression model (adjusted odds ratio, 2.39; 95% confidence interval [CI], 1.08 to 5.28; P=0.031). Total CAN score was positively associated with loguNAG (β=0.261, P=0.026) in the multivariate linear regression model. Log-uNAG was inversely correlated with frequency-domain and time-domain indices of HRV.
Conclusion
This study verified the association of uNAG with presence and severity of CAN and changes in HRV in T1DM patients without nephropathy. The potential role of uNAG should be further assessed for high-risk patients for CAN in T1DM patients without nephropathy. -
Citations
Citations to this article as recorded by- Determination of Diabetes-associated Cardiovascular Autonomic Neuropathy Risk Factors among Insulin and Non-insulin Dependent Diabetics
Ibrahim Abdulsada, Zain Alabdeen Obaid, Farah Almerza, Mays Alwaeli, Anmar Al-Elayawi, Taha Al-Dayyeni, Harir Al-Tuhafy
The Journal of Medical Research.2023; 9(6): 141. CrossRef - Association between carotid atherosclerosis and presence of intracranial atherosclerosis using three-dimensional high-resolution vessel wall magnetic resonance imaging in asymptomatic patients with type 2 diabetes
Ji Eun Jun, You-Cheol Hwang, Kyu Jeong Ahn, Ho Yeon Chung, Geon-Ho Jahng, Soonchan Park, In-Kyung Jeong, Chang-Woo Ryu
Diabetes Research and Clinical Practice.2022; 191: 110067. CrossRef
- Determination of Diabetes-associated Cardiovascular Autonomic Neuropathy Risk Factors among Insulin and Non-insulin Dependent Diabetics
- Response: An Electronic Health Record-Integrated Computerized Intravenous Insulin Infusion Protocol: Clinical Outcomes and
in Silico Adjustment (Diabetes Metab J 2020;44:56–66) - Sung Woon Park, Seunghyun Lee, Won Chul Cha, Kyu Yeon Hur, Jae Hyeon Kim, Moon-Kyu Lee, Sung-Min Park, Sang-Man Jin
- Diabetes Metab J. 2020;44(2):358-359. Published online April 23, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0080
- [Original]
- 4,054 View
- 58 Download
- Cardiovascular Risk/Epidemiology
- Validation of Risk Prediction Models for Atherosclerotic Cardiovascular Disease in a Prospective Korean Community-Based Cohort
- Jae Hyun Bae, Min Kyong Moon, Sohee Oh, Bo Kyung Koo, Nam Han Cho, Moon-Kyu Lee
- Diabetes Metab J. 2020;44(3):458-469. Published online January 13, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0061
- 6,868 View
- 226 Download
- 14 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background To investigate the performance of the 2013 American College of Cardiology/American Heart Association Pooled Cohort Equations (PCE) in a large, prospective, community-based cohort in Korea and to compare it with that of the Framingham Global Cardiovascular Disease Risk Score (FRS-CVD) and the Korean Risk Prediction Model (KRPM).
Methods In the Korean Genome and Epidemiology Study (KOGES)-Ansan and Ansung study, we evaluated calibration and discrimination of the PCE for non-Hispanic whites (PCE-WH) and for African Americans (PCE-AA) and compared their predictive abilities with the FRS-CVD and the KRPM.
Results The present study included 7,932 individuals (3,778 men and 4,154 women). The PCE-WH and PCE-AA moderately overestimated the risk of atherosclerotic cardiovascular disease (ASCVD) for men (6% and 13%, respectively) but underestimated the risk for women (−49% and −25%, respectively). The FRS-CVD overestimated ASCVD risk for men (91%) but provided a good risk prediction for women (3%). The KRPM underestimated ASCVD risk for men (−31%) and women (−31%). All the risk prediction models showed good discrimination in both men (C-statistic 0.730 to 0.735) and women (C-statistic 0.726 to 0.732). Recalibration of the PCE using data from the KOGES-Ansan and Ansung study substantially improved the predictive accuracy in men.
Conclusion In the KOGES-Ansan and Ansung study, the PCE overestimated ASCVD risk for men and underestimated the risk for women. The PCE-WH and the FRS-CVD provided an accurate prediction of ASCVD in men and women, respectively.
-
Citations
Citations to this article as recorded by- Risk Factors for Infertility in Korean Women
Juyeon Lee, Chang-Woo Choo, Kyoung Yong Moon, Sang Woo Lyu, Hoon Kim, Joong Yeup Lee, Jung Ryeol Lee, Byung Chul Jee, Kyungjoo Hwang, Seok Hyun Kim, Sue K. Park
Journal of Korean Medical Science.2024;[Epub] CrossRef - Evaluating cardiovascular disease risk stratification using multiple-polygenic risk scores and pooled cohort equations: insights from a 17-year longitudinal Korean cohort study
Yi Seul Park, Hye-Mi Jang, Ji Hye Park, Bong-Jo Kim, Hyun-Young Park, Young Jin Kim
Frontiers in Genetics.2024;[Epub] CrossRef - Moderation of Weight Misperception on the Associations Between Obesity Indices and Estimated Cardiovascular Disease Risk
Kayoung Lee
International Journal of Behavioral Medicine.2023; 30(1): 89. CrossRef - Validation of the general Framingham Risk Score (FRS), SCORE2, revised PCE and WHO CVD risk scores in an Asian population
Sazzli Shahlan Kasim, Nurulain Ibrahim, Sorayya Malek, Khairul Shafiq Ibrahim, Muhammad Firdaus Aziz, Cheen Song, Yook Chin Chia, Anis Safura Ramli, Kazuaki Negishi, Nafiza Mat Nasir
The Lancet Regional Health - Western Pacific.2023; 35: 100742. CrossRef - Principles of cardiovascular risk management in perimenopausal women with type 2 diabetes
F. O. Ushanova, T. Yu. Demidova, T. N. Korotkova
FOCUS. Endocrinology.2023; 4(2): 19. CrossRef - Prediction of the 10-year risk of atherosclerotic cardiovascular disease in the Korean population
Sangwoo Park, Yong-Giun Kim, Soe Hee Ann, Young-Rak Cho, Shin-Jae Kim, Seungbong Han, Gyung-Min Park
Epidemiology and Health.2023; 45: e2023052. CrossRef - Triglyceride-Glucose Index Predicts Future Atherosclerotic Cardiovascular Diseases: A 16-Year Follow-up in a Prospective, Community-Dwelling Cohort Study
Joon Ho Moon, Yongkang Kim, Tae Jung Oh, Jae Hoon Moon, Soo Heon Kwak, Kyong Soo Park, Hak Chul Jang, Sung Hee Choi, Nam H. Cho
Endocrinology and Metabolism.2023; 38(4): 406. CrossRef - Validity of the models predicting 10-year risk of cardiovascular diseases in Asia: A systematic review and prediction model meta-analysis
Mahin Nomali, Davood Khalili, Mehdi Yaseri, Mohammad Ali Mansournia, Aryan Ayati, Hossein Navid, Saharnaz Nedjat, Hean Teik Ong
PLOS ONE.2023; 18(11): e0292396. CrossRef - Assessing the Validity of the Criteria for the Extreme Risk Category of Atherosclerotic Cardiovascular Disease: A Nationwide Population-Based Study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Journal of Lipid and Atherosclerosis.2022; 11(1): 73. CrossRef - Mediation of Grip Strength on the Association Between Self-Rated Health and Estimated Cardiovascular Disease Risk
Kayoung Lee
Metabolic Syndrome and Related Disorders.2022; 20(6): 344. CrossRef - Implications of the heterogeneity between guideline recommendations for the use of low dose aspirin in primary prevention of cardiovascular disease
Xiao-Ying Li, Li Li, Sang-Hoon Na, Francesca Santilli, Zhongwei Shi, Michael Blaha
American Journal of Preventive Cardiology.2022; 11: 100363. CrossRef - The Risk of Cardiovascular Disease According to Chewing Status Could Be Modulated by Healthy Diet in Middle-Aged Koreans
Hyejin Chun, Jongchul Oh, Miae Doo
Nutrients.2022; 14(18): 3849. CrossRef - Management of Cardiovascular Risk in Perimenopausal Women with Diabetes
Catherine Kim
Diabetes & Metabolism Journal.2021; 45(4): 492. CrossRef - Comparative performance of the two pooled cohort equations for predicting atherosclerotic cardiovascular disease
Alessandra M. Campos-Staffico, David Cordwin, Venkatesh L. Murthy, Michael P. Dorsch, Jasmine A. Luzum
Atherosclerosis.2021; 334: 23. CrossRef - Usefulness of Relative Handgrip Strength as a Simple Indicator of Cardiovascular Risk in Middle-Aged Koreans
Won Bin Kim, Jun-Bean Park, Yong-Jin Kim
The American Journal of the Medical Sciences.2021; 362(5): 486. CrossRef
- Risk Factors for Infertility in Korean Women
- Drug/Regimen
-
- An Electronic Health Record-Integrated Computerized Intravenous Insulin Infusion Protocol: Clinical Outcomes and
in Silico Adjustment - Sung Woon Park, Seunghyun Lee, Won Chul Cha, Kyu Yeon Hur, Jae Hyeon Kim, Moon-Kyu Lee, Sung-Min Park, Sang-Man Jin
- Diabetes Metab J. 2020;44(1):56-66. Published online October 21, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0227
- 6,465 View
- 133 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background We aimed to describe the outcome of a computerized intravenous insulin infusion (CII) protocol integrated to the electronic health record (EHR) system and to improve the CII protocol
in silico using the EHR-based predictors of the outcome.Methods Clinical outcomes of the patients who underwent the CII protocol between July 2016 and February 2017 and their matched controls were evaluated. In the CII protocol group (
n =91), multivariable binary logistic regression analysis models were used to determine the independent associates with a delayed response (taking ≥6.0 hours for entering a glucose range of 70 to 180 mg/dL). The CII protocol was adjustedin silico according to the EHR-based parameters obtained in the first 3 hours of CII.Results Use of the CII protocol was associated with fewer subjects with hypoglycemia alert values (
P =0.003), earlier (P =0.002), and more stable (P =0.017) achievement of a glucose range of 70 to 180 mg/dL. Initial glucose level (P =0.001), change in glucose during the first 2 hours (P =0.026), and change in insulin infusion rate during the first 3 hours (P =0.029) were independently associated with delayed responses. Increasing the insulin infusion rate temporarily according to these parametersin silico significantly reduced delayed responses (P <0.0001) without hypoglycemia, especially in refractory patients.Conclusion Our CII protocol enabled faster and more stable glycemic control than conventional care with minimized risk of hypoglycemia. An EHR-based adjustment was simulated to reduce delayed responses without increased incidence of hypoglycemia.
-
Citations
Citations to this article as recorded by- Response: An Electronic Health Record-Integrated Computerized Intravenous Insulin Infusion Protocol: Clinical Outcomes and in Silico Adjustment (Diabetes Metab J 2020;44:56–66)
Sung Woon Park, Seunghyun Lee, Won Chul Cha, Kyu Yeon Hur, Jae Hyeon Kim, Moon-Kyu Lee, Sung-Min Park, Sang-Man Jin
Diabetes & Metabolism Journal.2020; 44(2): 358. CrossRef - Letter: An Electronic Health Record-Integrated Computerized Intravenous Insulin Infusion Protocol: Clinical Outcomes and in Silico Adjustment (Diabetes Metab J 2020;44:56–66)
Dongwon Yi
Diabetes & Metabolism Journal.2020; 44(2): 354. CrossRef
- Response: An Electronic Health Record-Integrated Computerized Intravenous Insulin Infusion Protocol: Clinical Outcomes and in Silico Adjustment (Diabetes Metab J 2020;44:56–66)
- Drug/Regimen
- Efficacy and Safety of Omega-3 Fatty Acids in Patients Treated with Statins for Residual Hypertriglyceridemia: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial
- Ji Eun Jun, In-Kyung Jeong, Jae Myung Yu, Sung Rae Kim, In Kye Lee, Kyung-Ah Han, Sung Hee Choi, Soo-Kyung Kim, Hyeong Kyu Park, Ji-Oh Mok, Yong-ho Lee, Hyuk-Sang Kwon, So Hun Kim, Ho-Cheol Kang, Sang Ah Lee, Chang Beom Lee, Kyung Mook Choi, Sung-Ho Her, Won Yong Shin, Mi-Seung Shin, Hyo-Suk Ahn, Seung Ho Kang, Jin-Man Cho, Sang-Ho Jo, Tae-Joon Cha, Seok Yeon Kim, Kyung Heon Won, Dong-Bin Kim, Jae Hyuk Lee, Moon-Kyu Lee
- Diabetes Metab J. 2020;44(1):78-90. Published online June 20, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0265
- 9,266 View
- 189 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Cardiovascular risk remains increased despite optimal low density lipoprotein cholesterol (LDL-C) level induced by intensive statin therapy. Therefore, recent guidelines recommend non-high density lipoprotein cholesterol (non-HDL-C) as a secondary target for preventing cardiovascular events. The aim of this study was to assess the efficacy and tolerability of omega-3 fatty acids (OM3-FAs) in combination with atorvastatin compared to atorvastatin alone in patients with mixed dyslipidemia.
Methods This randomized, double-blind, placebo-controlled, parallel-group, and phase III multicenter study included adults with fasting triglyceride (TG) levels ≥200 and <500 mg/dL and LDL-C levels <110 mg/dL. Eligible subjects were randomized to ATOMEGA (OM3-FAs 4,000 mg plus atorvastatin calcium 20 mg) or atorvastatin 20 mg plus placebo groups. The primary efficacy endpoints were the percent changes in TG and non-HDL-C levels from baseline at the end of treatment.
Results After 8 weeks of treatment, the percent changes from baseline in TG (−29.8% vs. 3.6%,
P <0.001) and non-HDL-C (−10.1% vs. 4.9%,P <0.001) levels were significantly greater in the ATOMEGA group (n =97) than in the atorvastatin group (n =103). Moreover, the proportion of total subjects reaching TG target of <200 mg/dL in the ATOMEGA group was significantly higher than that in the atorvastatin group (62.9% vs. 22.3%,P <0.001). The incidence of adverse events did not differ between the two groups.Conclusion The addition of OM3-FAs to atorvastatin improved TG and non-HDL-C levels to a significant extent compared to atorvastatin alone in subjects with residual hypertriglyceridemia.
-
Citations
Citations to this article as recorded by- Association Between Omega‐3 Fatty Acid Intake and Dyslipidemia: A Continuous Dose–Response Meta‐Analysis of Randomized Controlled Trials
Tianjiao Wang, Xin Zhang, Na Zhou, Yuxuan Shen, Biao Li, Bingshu E. Chen, Xinzhi Li
Journal of the American Heart Association.2023;[Epub] CrossRef - Nutraceutical support in the prevention and treatment of cardiovascular diseases
E. V. Gracheva, E. A. Starovoytova, E. S. Kulikov, N. A. Kirillova, S. V. Fedosenko, M. A. Balaganskaya, D. V. Kromka
Rational Pharmacotherapy in Cardiology.2023; 19(3): 298. CrossRef - Effect of coadministration of omega-3 fatty acids with glimepiride on glycemic control, lipid profile, irisin, and sirtuin-1 in type 2 diabetes mellitus patients: a randomized controlled trial
Rehab H. Werida, Aalaa Ramzy, Youssri Nassief Ebrahim, Maged Wasfy Helmy
BMC Endocrine Disorders.2023;[Epub] CrossRef - The Effect of Dietary Interventions on Hypertriglyceridemia: From Public Health to Molecular Nutrition Evidence
Karla Paulina Luna-Castillo, Xochitl Citlalli Olivares-Ochoa, Rocío Guadalupe Hernández-Ruiz, Iris Monserrat Llamas-Covarrubias, Saraí Citlalic Rodríguez-Reyes, Alejandra Betancourt-Núñez, Barbara Vizmanos, Erika Martínez-López, José Francisco Muñoz-Valle
Nutrients.2022; 14(5): 1104. CrossRef - The effect of omega-3 fatty acids and its combination with statins on lipid profile in patients with hypertriglyceridemia: A systematic review and meta-analysis of randomized controlled trials
Yunjiao Yang, Wen Deng, Yanmei Wang, Tongyi Li, Yiding Chen, Cong Long, Qing Wen, Yue Wu, Qiu Chen
Frontiers in Nutrition.2022;[Epub] CrossRef - Comparison of the Efficacy and Safety of Atorvastatin 40 mg/ω-3 Fatty Acids 4 g Fixed-dose Combination and Atorvastatin 40 mg Monotherapy in Hypertriglyceridemic Patients who Poorly Respond to Atorvastatin 40 mg Monotherapy: An 8-week, Multicenter, Random
Jong Shin Woo, Soon Jun Hong, Dong Hoon Cha, Kee Sik Kim, Moo Hyun Kim, Jun-Won Lee, Myung Ho Jeong, Jin-Ok Jeong, Jun-Hee Lee, Doo Soo Jeon, Eun Joo Cho, Soon Kil Kim, Jun Kwan, Chang Gyu Park, Hae Young Lee, Taek Jong Hong, Jinho Shin, Ho Joong Youn, Do
Clinical Therapeutics.2021; 43(8): 1419. CrossRef - All-Cause Mortality and Cardiovascular Death between Statins and Omega-3 Supplementation: A Meta-Analysis and Network Meta-Analysis from 55 Randomized Controlled Trials
Jeongseon Kim, Tung Hoang, Ji-Myung Kim, So Young Bu, Jeong-Hwa Choi, Eunju Park, Seung-Min Lee, Eunmi Park, Ji Yeon Min, In Seok Lee, So Young Youn, Jee-Young Yeon
Nutrients.2020; 12(10): 3203. CrossRef
- Association Between Omega‐3 Fatty Acid Intake and Dyslipidemia: A Continuous Dose–Response Meta‐Analysis of Randomized Controlled Trials
- Clinical Diabetes & Therapeutics
- Additional Effect of Dietary Fiber in Patients with Type 2 Diabetes Mellitus Using Metformin and Sulfonylurea: An Open-Label, Pilot Trial
- Seung-Eun Lee, Yongbin Choi, Ji Eun Jun, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Gwang Pyo Ko, Moon-Kyu Lee
- Diabetes Metab J. 2019;43(4):422-431. Published online April 23, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0090
- 5,785 View
- 77 Download
- 8 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Metformin, sulfonylurea, and dietary fiber are known to affect gut microbiota in patients with type 2 diabetes mellitus (T2DM). This open and single-arm pilot trial investigated the effects of the additional use of fiber on glycemic parameters, insulin, incretins, and microbiota in patients with T2DM who had been treated with metformin and sulfonylurea.
Methods Participants took fiber for 4 weeks and stopped for the next 4 weeks. Glycemic parameters, insulin, incretins during mixed-meal tolerance test (MMTT), lipopolysaccharide (LPS) level, and fecal microbiota were analyzed at weeks 0, 4, and 8. The first tertile of difference in glucose area under the curve during MMTT between weeks 0 and 4 was defined as ‘responders’ and the third as ‘nonresponders,’ respectively.
Results In all 10 participants, the peak incretin levels during MMTT were higher and LPS were lower at week 4 as compared with at baseline. While the insulin sensitivity of the ‘responders’ increased at week 4, that of the ‘nonresponders’ showed opposite results. However, the results were not statistically significant. In all participants, metabolically unfavorable microbiota decreased at week 4 and were restored at week 8. At baseline, metabolically hostile bacteria were more abundant in the ‘nonresponders.’ In ‘responders,’
Roseburia intestinalis increased at week 4.Conclusion While dietary fiber did not induce additional changes in glycemic parameters, it showed a trend of improvement in insulin sensitivity in ‘responders.’ Even if patients are already receiving diabetes treatment, the additional administration of fiber can lead to additional benefits in the treatment of diabetes.
-
Citations
Citations to this article as recorded by- The effects of prebiotics on gastrointestinal side effects of metformin in youth: A pilot randomized control trial in youth-onset type 2 diabetes
Sydney A. Dixon, Sidharth Mishra, Katrina B. Dietsche, Shalini Jain, Lilian Mabundo, Michael Stagliano, Andrea Krenek, Amber Courville, Shanna Yang, Sara A. Turner, Abby G. Meyers, Doris E. Estrada, Hariom Yadav, Stephanie T. Chung
Frontiers in Endocrinology.2023;[Epub] CrossRef - The impact of dietary, surgical, and pharmacological interventions on gut microbiota in individuals with diabetes mellitus: A systematic review
Patricia M. Bock, Andreza F. Martins, Rafaela Ramalho, Gabriela H. Telo, Gabriel Leivas, Clara K. Maraschin, Beatriz D. Schaan
Diabetes Research and Clinical Practice.2022; 189: 109944. CrossRef - Assessment of the safety and probiotic properties of Roseburia intestinalis: A potential “Next Generation Probiotic”
Chao Zhang, Kejia Ma, Kai Nie, Minzi Deng, Weiwei Luo, Xing Wu, Yujun Huang, Xiaoyan Wang
Frontiers in Microbiology.2022;[Epub] CrossRef - The Effect of Prebiotics and Oral Anti-Diabetic Agents on Gut Microbiome in Patients with Type 2 Diabetes: A Systematic Review and Network Meta-Analysis of Randomised Controlled Trials
Omorogieva Ojo, Xiaohua Wang, Osarhumwese Osaretin Ojo, Joanne Brooke, Yiqing Jiang, Qingqing Dong, Trevor Thompson
Nutrients.2022; 14(23): 5139. CrossRef - The Effect of Dietary Interventions on Chronic Inflammatory Diseases in Relation to the Microbiome: A Systematic Review
Carlijn A. Wagenaar, Marieke van de Put, Michelle Bisschops, Wendy Walrabenstein, Catharina S. de Jonge, Hilde Herrema, Dirkjan van Schaardenburg
Nutrients.2021; 13(9): 3208. CrossRef - The Role of Dietary Fibre in Modulating Gut Microbiota Dysbiosis in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomised Controlled Trials
Omorogieva Ojo, Qian-Qian Feng, Osarhumwese Osaretin Ojo, Xiao-Hua Wang
Nutrients.2020; 12(11): 3239. CrossRef - High Fiber and Beta Carotene from Sweet Potatoes and Pumpkin Improve Insulin Resistance by Inhibition of Sterol Regulatory Binding Protein 1c in Liver of Hypertriglyceridemic Rats
Sunarti Sunarti, Umar Santoso, Abrory Agus Cahya Pramana, Emy Huriyati, Dianandha Septiana Rubi
Open Access Macedonian Journal of Medical Sciences.2020; 8(A): 898. CrossRef
- The effects of prebiotics on gastrointestinal side effects of metformin in youth: A pilot randomized control trial in youth-onset type 2 diabetes
- Obesity and Metabolic Syndrome
- The Protective Effects of Increasing Serum Uric Acid Level on Development of Metabolic Syndrome
- Tae Yang Yu, Sang-Man Jin, Jae Hwan Jee, Ji Cheol Bae, Moon-Kyu Lee, Jae Hyeon Kim
- Diabetes Metab J. 2019;43(4):504-520. Published online February 21, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0079
- 4,707 View
- 52 Download
- 14 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background It has not been determined whether changes in serum uric acid (SUA) level are associated with incident metabolic syndrome (MetS). The aim of the current study was to investigate the relationship between changes in SUA level and development of MetS in a large number of subjects.
Methods In total, 13,057 subjects participating in a medical health check-up program without a diagnosis of MetS at baseline were enrolled. Cox proportional hazards models were used to test the independent association of percent changes in SUA level with development of MetS.
Results After adjustment for age, systolic blood pressure, body mass index, fat-free mass (%), estimated glomerular filtration rate, smoking status, fasting glucose, triglyceride, low density lipoprotein cholesterol, high density lipoprotein cholesterol, and baseline SUA levels, the hazard ratios (HRs) (95% confidence intervals [CIs]) for incident MetS in the second, third, and fourth quartiles compared to the first quartile of percent change in SUA level were 1.055 (0.936 to 1.190), 0.927 (0.818 to 1.050), and 0.807 (0.707 to 0.922) in male (
P for trend <0.001) and 1.000 (0.843 to 1.186), 0.744 (0.615 to 0.900), and 0.684 (0.557 to 0.840) in female (P for trend <0.001), respectively. As a continuous variable in the fully-adjusted model, each one-standard deviation increase in percent change in SUA level was associated with an HR (95% CI) for incident MetS of 0.944 (0.906 to 0.982) in male (P =0.005) and 0.851 (0.801 to 0.905) in female (P <0.001).Conclusion The current study demonstrated that increasing SUA level independently protected against the development of MetS, suggesting a possible role of SUA as an antioxidant in the pathogenesis of incident MetS.
-
Citations
Citations to this article as recorded by- High prevalence of hyperuricemia and the association with metabolic syndrome in the rural areas of Southwestern China: A structural equation modeling based on the Zhuang minority cohort
Xiaofen Tang, Shun Liu, Xiaoqiang Qiu, Li Su, Dongping Huang, Jun Liang, Yu Yang, Jennifer Hui Juan Tan, Xiaoyun Zeng, Yihong Xie
Nutrition, Metabolism and Cardiovascular Diseases.2024; 34(2): 497. CrossRef - Predictive Value of Collagen Biomarkers in Advanced Chronic Kidney Disease Patients
Carina Ureche, Gianina Dodi, Adela Mihaela Șerban, Andreea Simona Covic, Luminița Voroneanu, Simona Hogaș, Radu Andy Sascău, Cristian Stătescu, Adrian Covic
Biomolecules.2023; 13(2): 389. CrossRef - The bidirectional relationship between metabolic syndrome and hyperuricemia in China: A longitudinal study from CHARLS
Wen-Yu Chen, Yan-Peng Fu, Min Zhou
Endocrine.2022; 76(1): 62. CrossRef - Correlation between Serum Oxidative Stress Level and Serum Uric Acid and Prognosis in Patients with Hepatitis B-Related Liver Cancer before Operation
Maowen Yu, Chaozhu Zhang, Hongbo Tang, Chaohui Xiao, Hangjun Che
Journal of Healthcare Engineering.2022; 2022: 1. CrossRef - Association between metabolic syndrome and uric acid: a systematic review and meta-analysis
Elena Raya-Cano, Manuel Vaquero-Abellán, Rafael Molina-Luque, Domingo De Pedro-Jiménez, Guillermo Molina-Recio, Manuel Romero-Saldaña
Scientific Reports.2022;[Epub] CrossRef - Acute moderate‐intensity aerobic exercise promotes purinergic and inflammatory responses in sedentary, overweight and physically active subjects
Cesar Eduardo Jacintho Moritz, Franccesco Pinto Boeno, Alexandra Ferreira Vieira, Samuel Vargas Munhoz, Juliete Nathali Scholl, Amanda de Fraga Dias, Pauline Rafaela Pizzato, Fabrício Figueiró, Ana Maria Oliveira Battastini, Alvaro Reischak‐Oliveira
Experimental Physiology.2021; 106(4): 1024. CrossRef - Association between baseline and changes in serum uric acid and incident metabolic syndrome: a nation-wide cohort study and updated meta-analysis
Sen Chen, Nianwei Wu, Chuan Yu, Ying Xu, Chengfu Xu, Yuli Huang, Jian Zhao, Ningxiu Li, Xiong-Fei Pan
Nutrition & Metabolism.2021;[Epub] CrossRef - Can biomarkers be used to improve diagnosis and prediction of metabolic syndrome in childhood cancer survivors? A systematic review
Vincent G. Pluimakers, Selveta S. van Santen, Marta Fiocco, Marie‐Christine E. Bakker, Aart J. van der Lelij, Marry M. van den Heuvel‐Eibrink, Sebastian J. C. M. M. Neggers
Obesity Reviews.2021;[Epub] CrossRef - Inverse associations between serum urate and glycemic status in a general population and in persons with diabetes mellitus
Ichiro Wakabayashi
Diabetology & Metabolic Syndrome.2020;[Epub] CrossRef - Association of Serum Uric Acid with Metabolic Syndrome and Its Components: A Mendelian Randomization Analysis
Lu Wang, Tao Zhang, Yafei Liu, Fang Tang, Fuzhong Xue
BioMed Research International.2020; 2020: 1. CrossRef - Association between Serum Uric Acid and Metabolic Syndrome in Koreans
Jihyun Jeong, Young Ju Suh
Journal of Korean Medical Science.2019;[Epub] CrossRef
- High prevalence of hyperuricemia and the association with metabolic syndrome in the rural areas of Southwestern China: A structural equation modeling based on the Zhuang minority cohort
- Epidemiology
- Diabetes Fact Sheet in Korea, 2016: An Appraisal of Current Status
- Jong Chul Won, Jae Hyuk Lee, Jae Hyeon Kim, Eun Seok Kang, Kyu Chang Won, Dae Jung Kim, Moon-Kyu Lee
- Diabetes Metab J. 2018;42(5):415-424. Published online August 9, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0017
- 8,866 View
- 89 Download
- 72 Web of Science
- 72 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background This report presents the recent prevalence and comorbidities related to diabetes in Korea by analyzing the nationally representative data.
Methods Using data from the Korea National Health and Nutrition Examination Survey for 2013 to 2014, the percentages and the total number of subjects over the age of 30 years with diabetes and prediabetes were estimated and applied to the National Population Census in 2014. Diagnosis of diabetes was based on fasting plasma glucose (≥126 mg/dL), current taking of antidiabetic medication, history of previous diabetes, or glycosylated hemoglobin (HbA1c) ≥6.5%. Impaired fasting glucose (IFG) was defined by fasting plasma glucose in the range of 100 to 125 mg/dL among those without diabetes.
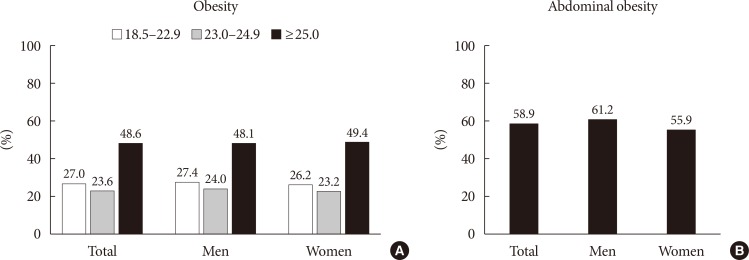
Results About 4.8 million (13.7%) Korean adults (≥30 years old) had diabetes, and about 8.3 million (24.8%) Korean adults had IFG. However, 29.3% of the subjects with diabetes are not aware of their condition. Of the subjects with diabetes, 48.6% and 54.7% were obese and hypertensive, respectively, and 31.6% had hypercholesterolemia. Although most subjects with diabetes (89.1%) were under medical treatment, and mostly being treated with oral hypoglycemic agents (80.2%), 10.8% have remained untreated. With respect to overall glycemic control, 43.5% reached the target of HbA1c <7%, whereas 23.3% reached the target when the standard was set to HbA1c <6.5%, according to the Korean Diabetes Association guideline.
Conclusion Diabetes is a major public health threat in Korea, but a significant proportion of adults were not controlling their illness. We need comprehensive approaches to overcome the upcoming diabetes-related disease burden in Korea.
-
Citations
Citations to this article as recorded by- Impact of anaerobic zone on biodegradation of micropollutants: Comparison of micropollutants’ removal efficiencies in lab-scale anaerobic bioreactor and in full-scale anaerobic zone
Jingyeong Shin, Sungman Lee, Jihea Lee, Heejong Son, Yunho Lee, Young Mo Kim
Chemical Engineering Journal.2024; 481: 148356. CrossRef - Clinical traits and systemic risks of familial diabetes mellitus according to age of onset and quantity:
an analysis of data from the community-based KoGES cohort study
Ju-Yeun Lee, Kyungsik Kim, Sangjun Lee, Woo Ju An, Sue K. Park
Epidemiology and Health.2023; 45: e2023029. CrossRef - The prevalence and predictors of pre-diabetes and diabetes among adults 40–70 years in Kharameh cohort study: A population-based study in Fars province, south of Iran
Masoumeh Ghoddusi Johari, Kimia Jokari, Alireza Mirahmadizadeh, Mozhgan Seif, Abbas Rezaianzadeh
Journal of Diabetes & Metabolic Disorders.2022; 21(1): 85. CrossRef - Concept and Proof of the Lifelog Bigdata Platform for Digital Healthcare and Precision Medicine on the Cloud
Kyu Hee Lee, Erdenebayar Urtnasan, Sangwon Hwang, Hee Young Lee, Jung Hun Lee, Sang Baek Koh, Hyun Youk
Yonsei Medical Journal.2022; 63(Suppl): S84. CrossRef - The Impact of Diabetes on Vascular Disease: Progress from the Perspective of Epidemics and Treatments
Runyang Liu, Lihua Li, Chen Shao, Honghua Cai, Zhongqun Wang, Pawel Kleczynski
Journal of Diabetes Research.2022; 2022: 1. CrossRef - Incidence and Predisposing Factors of Postoperative Infection after Rhinoplasty: A Single Surgeon’s 16-Year Experience with 2630 Cases in an East Asian Population
Khanh Ngoc Tran, Yong Ju Jang
Plastic & Reconstructive Surgery.2022; 150(1): 51e. CrossRef - Predictors for successful weight reduction during treatment with Dapagliflozin among patients with type 2 diabetes mellitus in primary care
Youn Huh, Young Sik Kim
BMC Primary Care.2022;[Epub] CrossRef - Skin accumulation of advanced glycation end products and cardiovascular risk in Korean patients with type 2 diabetes mellitus
Lee-Seoul Choi, Kainat Ahmed, Young-Seol Kim, Jung-Eun Yim
Heliyon.2022; 8(6): e09571. CrossRef - Health-related Quality of Life Instrument With 8 Items for Use in Patients With Type 2 Diabetes Mellitus: A Validation Study in Korea
Juyoung Kim, Hyeon-Jeong Lee, Min-Woo Jo
Journal of Preventive Medicine and Public Health.2022; 55(3): 234. CrossRef - Factors Influencing the Utilization of Diabetes Complication Tests Under the COVID-19 Pandemic: Machine Learning Approach
Haewon Byeon
Frontiers in Endocrinology.2022;[Epub] CrossRef - Prevalence and risk of diabetic complications in young-onset versus late-onset type 2 diabetes mellitus
Yongin Cho, Hye-Sun Park, Byung Wook Huh, Seong Ha Seo, Da Hea Seo, Seong Hee Ahn, Seongbin Hong, Young Ju Suh, So Hun Kim
Diabetes & Metabolism.2022; 48(6): 101389. CrossRef - Prevalence and Early Prediction of Diabetes Using Machine Learning in North Kashmir: A Case Study of District Bandipora
Salliah Shafi Bhat, Venkatesan Selvam, Gufran Ahmad Ansari, Mohd Dilshad Ansari, Md Habibur Rahman, Mamoon Rashid
Computational Intelligence and Neuroscience.2022; 2022: 1. CrossRef - Association between Nighttime Work and HbA1c Levels in South Korea
Yeon-Suk Lee, Jae Hong Joo, Eun-Cheol Park
Healthcare.2022; 10(10): 1977. CrossRef - Differences in health behavior and nutrient intake status between diabetes-aware and unaware Korean adults based on the Korea national health and nutrition examination survey 2016–18 data: A cross-sectional study
Anshul Sharma, Chen Lulu, Kee-Ho Song, Hae-Jeung Lee
Frontiers in Public Health.2022;[Epub] CrossRef - Screening for Prediabetes and Diabetes in Korean Nonpregnant Adults: A Position Statement of the Korean Diabetes Association, 2022
Kyung Ae Lee, Dae Jung Kim, Kyungdo Han, Suk Chon, Min Kyong Moon
Diabetes & Metabolism Journal.2022; 46(6): 819. CrossRef - Sex differences in sarcopenia and frailty among community‐dwelling Korean older adults with diabetes: The Korean Frailty and Aging Cohort Study
Sunyoung Kang, Tae Jung Oh, Be Long Cho, Yong Soon Park, Eun Roh, Hyeon Ju Kim, Sam‐Gyu Lee, Bong Jo Kim, Miji Kim, Chang Won Won, Hak Chul Jang
Journal of Diabetes Investigation.2021; 12(2): 155. CrossRef - Umbilical Cord-Mesenchymal Stem Cell-Conditioned Medium Improves Insulin Resistance in C2C12 Cell
Kyung-Soo Kim, Yeon Kyung Choi, Mi Jin Kim, Jung Wook Hwang, Kyunghoon Min, Sang Youn Jung, Soo-Kyung Kim, Yong-Soo Choi, Yong-Wook Cho
Diabetes & Metabolism Journal.2021; 45(2): 260. CrossRef - Hemoglobin glycation index is associated with incident chronic kidney disease in subjects with impaired glucose metabolism: A 10-year longitudinal cohort study
Wonjin Kim, Taehwa Go, Dae Ryong Kang, Eun Jig Lee, Ji Hye Huh
Journal of Diabetes and its Complications.2021; 35(1): 107760. CrossRef - East Asian diet‐mimicking diet plan based on the Mediterranean diet and the Dietary Approaches to Stop Hypertension diet in adults with type 2 diabetes: A randomized controlled trial
Sang‐Man Jin, Jiyeon Ahn, Jiyun Park, Kyu Yeon Hur, Jae Hyeon Kim, Moon‐Kyu Lee
Journal of Diabetes Investigation.2021; 12(3): 357. CrossRef - Status of Diabetic Neuropathy in Korea: A National Health Insurance Service-National Sample Cohort Analysis (2006 to 2015)
Seong-Su Moon, Chong Hwa Kim, Seon Mee Kang, Eun Sook Kim, Tae Jung Oh, Jae-Seung Yun, Ho Chan Cho, Dae Jung Kim, Tae Sun Park
Diabetes & Metabolism Journal.2021; 45(1): 115. CrossRef - Diabetes Fact Sheets in Korea, 2020: An Appraisal of Current Status
Chan-Hee Jung, Jang Won Son, Shinae Kang, Won Jun Kim, Hun-Sung Kim, Hae Soon Kim, Mihae Seo, Hye-Jung Shin, Seong-Su Lee, Su Jin Jeong, Yongin Cho, Seung Jin Han, Hyang Mi Jang, Mira Rho, Shinbi Lee, Mihyun Koo, Been Yoo, Jung-Wha Moon, Hye Young Lee, Ja
Diabetes & Metabolism Journal.2021; 45(1): 1. CrossRef - Considering serum alanine aminotransferase and gamma-glutamyltransferase levels together strengthen the prediction of impaired fasting glucose risk: a cross-sectional and longitudinal study
Ji Hye Jeong, Susie Jung, Kyu-Nam Kim
Scientific Reports.2021;[Epub] CrossRef - The Associations Between Vitamin D Receptor BsmI and ApaI Polymorphisms and Obesity in Korean Patients with Type 2 Diabetes Mellitus
Sang Won Nam, Jinwoo Choi, Hyun Jeong Jeon, Tae Keun Oh, Dong-Hwa Lee
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 557. CrossRef - Association between living alone and incident type 2 diabetes among middle-aged individuals in Korea: a nationwide cohort study
Ga Eun Nam, Wonsock Kim, Kyungdo Han, Jin-Hyung Jung, Byoungduck Han, Jinwook Kim, Nan Hee Kim, Kyung Mook Choi, Kyung Hwan Cho, Yong Gyu Park, Seon Mee Kim
Scientific Reports.2021;[Epub] CrossRef - Retracted: Western pacific consensus proposals for management of prediabetes
International Journal of Clinical Practice.2021;[Epub] CrossRef - Blood glucose levels and bodyweight change after dapagliflozin administration
Hyunah Kim, Seung‐Hwan Lee, Hyunyong Lee, Hyeon Woo Yim, Jae‐Hyoung Cho, Kun‐Ho Yoon, Hun‐Sung Kim
Journal of Diabetes Investigation.2021; 12(9): 1594. CrossRef - Prevalence and socioeconomic burden of diabetes mellitus in South Korean adults: a population-based study using administrative data
Sung-Hee Oh, Hyemin Ku, Kang Seo Park
BMC Public Health.2021;[Epub] CrossRef - Prediction of Type 2 Diabetes Based on Machine Learning Algorithm
Henock M. Deberneh, Intaek Kim
International Journal of Environmental Research and Public Health.2021; 18(6): 3317. CrossRef - Development of a clinical risk score for incident diabetes: A 10‐year prospective cohort study
Tae Jung Oh, Jae Hoon Moon, Sung Hee Choi, Young Min Cho, Kyong Soo Park, Nam H Cho, Hak Chul Jang
Journal of Diabetes Investigation.2021; 12(4): 610. CrossRef - New Era for Renal-Protective Therapy in Type 2 Diabetes: Better Renal Outcomes in Patients with Type 2 Diabetes Taking Sodium-Glucose Cotransporter 2 Inhibitors versus Dipeptidyl Peptidase-4 Inhibitors
Chan-Hee Jung
Endocrinology and Metabolism.2021; 36(2): 339. CrossRef - Treatment Patterns of Type 2 Diabetes Assessed Using a Common Data Model Based on Electronic Health Records of 2000–2019
Kyung Ae Lee, Heung Yong Jin, Yu Ji Kim, Yong-Jin Im, Eun-Young Kim, Tae Sun Park
Journal of Korean Medical Science.2021;[Epub] CrossRef - No influence of hepatic steatosis on the 3‐year outcomes of patients with quiescent chronic hepatitis B
Jin Won Chang, Jae Seung Lee, Hye Won Lee, Beom Kyung Kim, Jun Yong Park, Do Young Kim, Sang Hoon Ahn, Seung Up Kim
Journal of Viral Hepatitis.2021; 28(11): 1545. CrossRef - Occupational Noise Exposure and Incidence of High Fasting Blood Glucose: A 3-Year, Multicenter, Retrospective Study
Seunghan Kim, Byungyoon Yun, Seunghyun Lee, Changyoung Kim, Juho Sim, Ara Cho, Yeonsuh Oh, Jiho Lee, Jinha Yoon
International Journal of Environmental Research and Public Health.2021; 18(17): 9388. CrossRef - Young-onset type 2 diabetes in South Korea: a review of the current status and unmet need
Ye Seul Yang, Kyungdo Han, Tae Seo Sohn, Nam Hoon Kim
The Korean Journal of Internal Medicine.2021; 36(5): 1049. CrossRef - Blood Pressure and Cardiovascular Disease in Older Patients With Diabetes: Retrospective Cohort Study
Sangmo Hong, Jung Hwan Park, Kyungdo Han, Chang Beom Lee, Dong Sun Kim, Sung Hoon Yu
Journal of the American Heart Association.2021;[Epub] CrossRef - Prevalence of significant hepatic fibrosis using magnetic resonance elastography in a health check‐up clinic population
Kyung A Kang, Dae Won Jun, Mi Sung Kim, Heon‐Ju Kwon, Mindie H. Nguyen
Alimentary Pharmacology & Therapeutics.2020; 51(3): 388. CrossRef - The Effects of Bariatric Surgery on Type 2 Diabetes in Asian Populations: a Meta-analysis of Randomized Controlled Trials
Jin Hwa Kim, Jung-Soo Pyo, Won Jin Cho, Sang Yong Kim
Obesity Surgery.2020; 30(3): 910. CrossRef - Opposite Effects of Work-Related Physical Activity and Leisure-Time Physical Activity on the Risk of Diabetes in Korean Adults
Hyun Sook Oh
International Journal of Environmental Research and Public Health.2020; 17(16): 5812. CrossRef - Middle-aged men with type 2 diabetes as potential candidates for pancreatic cancer screening: a 10-year nationwide population-based cohort study
Dong-Hoe Koo, Kyung-Do Han, Hong Joo Kim, Cheol-Young Park
Acta Diabetologica.2020; 57(2): 197. CrossRef - Efficacy and safety of insulin glargine 300 U/mL versus insulin glargine 100 U/mL in Asia Pacific insulin‐naïve people with type 2 diabetes: The EDITION AP randomized controlled trial
Linong Ji, Eun Seok Kang, XiaoLin Dong, Ling Li, GuoYue Yuan, Shuhua Shang, Elisabeth Niemoeller
Diabetes, Obesity and Metabolism.2020; 22(4): 612. CrossRef - Non-Exercise Based Estimation of Cardiorespiratory Fitness Mediates Associations between Comorbidities and Health-Related Quality of Life in Older Korean Adults with Diabetes
Inhwan Lee, Shinuk Kim, Hyunsik Kang
International Journal of Environmental Research and Public Health.2020; 17(4): 1164. CrossRef - γ-Linolenic Acid versus α-Lipoic Acid for Treating Painful Diabetic Neuropathy in Adults: A 12-Week, Double-Placebo, Randomized, Noninferiority Trial
Jong Chul Won, Hyuk-Sang Kwon, Seong-Su Moon, Sung Wan Chun, Chong Hwa Kim, Ie Byung Park, In Joo Kim, Jihyun Lee, Bong Yun Cha, Tae Sun Park
Diabetes & Metabolism Journal.2020; 44(4): 542. CrossRef - Circulating myokine levels in different stages of glucose intolerance
Kahui Park, Chul Woo Ahn, Jong Suk Park, YuSik Kim, Ji Sun Nam
Medicine.2020; 99(8): e19235. CrossRef - Associations among Obesity Degree, Glycemic Status, and Risk of Heart Failure in 9,720,220 Korean Adults
Eun-Jung Rhee, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Yang-Hyun Kim, Won-Young Lee
Diabetes & Metabolism Journal.2020; 44(4): 592. CrossRef - The sweet spot: fasting glucose, cardiovascular disease, and mortality in older adults with diabetes: a nationwide population-based study
Ji Hyun Lee, Kyungdo Han, Ji Hye Huh
Cardiovascular Diabetology.2020;[Epub] CrossRef - Glucose-Lowering Effect of Home-Delivered Therapeutic Meals in Patients with Type 2 Diabetes
Jong Han Choi, Se Hee Min, Kyeong Hye Lim, Uoon Jeong Shin, Min-Seon Kim
The Journal of Korean Diabetes.2020; 21(1): 46. CrossRef - Fasting Plasma Glucose Level Independently Predicts the Mortality of Patients with Coronavirus Disease 2019 Infection: A Multicenter, Retrospective Cohort Study
Min Cheol Chang, Jong-Moon Hwang, Jae-Han Jeon, Sang Gyu Kwak, Donghwi Park, Jun Sung Moon
Endocrinology and Metabolism.2020; 35(3): 595. CrossRef - Gender differences in adverse event reports associated with antidiabetic drugs
Kyung-In Joung, Gyu-Won Jung, Han-Heui Park, Hyesung Lee, So-Hee Park, Ju-Young Shin
Scientific Reports.2020;[Epub] CrossRef - Relative fat mass at baseline and its early change may be a predictor of incident nonalcoholic fatty liver disease
Hwi Young Kim, Su Jung Baik, Hye Ah Lee, Byoung Kwon Lee, Hye Sun Lee, Tae Hun Kim, Kwon Yoo
Scientific Reports.2020;[Epub] CrossRef - Peripheral Arterial Stiffness Increases the Risk of Progression of Renal Disease in Type 2 Diabetic Patients
Tae Hoon Lim, Seung Min Chung, Dong Sung Lee, Se Ra Choi, Jun Sung Moon, Ji Sung Yoon, Kyu Chang Won, Hyoung Woo Lee
Frontiers in Medicine.2020;[Epub] CrossRef Association of Urinary Polycyclic Aromatic Hydrocarbons and Diabetes in Korean Adults: Data from the Korean National Environmental Health Survey Cycle 2 (2012–2014)
Yon Ju Nam, Shin-Hye Kim
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 3993. CrossRef- Present and Future of Digital Health in Diabetes and Metabolic Disease
Sang Youl Rhee, Chiweon Kim, Dong Wook Shin, Steven R. Steinhubl
Diabetes & Metabolism Journal.2020; 44(6): 819. CrossRef - Trends in the Incidence, Prevalence, and Mortality of End-Stage Kidney Disease in South Korea
Min-Jeong Lee, Kyoung Hwa Ha, Dae Jung Kim, Inwhee Park
Diabetes & Metabolism Journal.2020; 44(6): 933. CrossRef - An evaluation of the impact of aggressive diabetes and hypertension management on chronic kidney diseases at the population level: a simulation analysis
John Pastor Ansah, Shawn Tan Yi Wei, Tessa Lui Shi Min
System Dynamics Review.2020; 36(4): 497. CrossRef - Nationwide Trends in Pancreatitis and Pancreatic Cancer Risk Among Patients With Newly Diagnosed Type 2 Diabetes Receiving Dipeptidyl Peptidase 4 Inhibitors
Minyoung Lee, Jiyu Sun, Minkyung Han, Yongin Cho, Ji-Yeon Lee, Chung Mo Nam, Eun Seok Kang
Diabetes Care.2019; 42(11): 2057. CrossRef - Clinical Efficacy and Parameters Affecting the Response to Dulaglutide Treatment in Patients with Type 2 Diabetes: A Retrospective, Real-World Data Study
Jee Hee Yoo, Yun Kyung Cho, Jiwoo Lee, Hwi Seung Kim, Yu Mi Kang, Chang Hee Jung, Joong-Yeol Park, Woo Je Lee
Diabetes Therapy.2019; 10(4): 1453. CrossRef - Diabetes and the Risk of Infection: A National Cohort Study
Eun Jin Kim, Kyoung Hwa Ha, Dae Jung Kim, Young Hwa Choi
Diabetes & Metabolism Journal.2019; 43(6): 804. CrossRef - Current Management of Type 2 Diabetes Mellitus in Primary Care Clinics in Korea
Da Hea Seo, Shinae Kang, Yong-ho Lee, Jung Yoon Ha, Jong Suk Park, Byoung-Wan Lee, Eun Seok Kang, Chul Woo Ahn, Bong-Soo Cha
Endocrinology and Metabolism.2019; 34(3): 282. CrossRef - Effects of Blood Pressure and Glucose Levels on Visual Acuity
Dae-Jong Kim
Journal of Korean Ophthalmic Optics Society.2019; 24(2): 181. CrossRef - An evaluation of the impact of aggressive hypertension, diabetes and smoking cessation management on CVD outcomes at the population level: a dynamic simulation analysis
John Pastor Ansah, Ryan Leung Hoe Inn, Salman Ahmad
BMC Public Health.2019;[Epub] CrossRef -
Retracted
: Angelica polysaccharide alleviates TNF‐α‐induced MIN6 cell damage a through the up‐regulation microRNA‐143
Yingying Zhao, Chuanqian Liu, Xueting Zhang, Xipeng Yan
BioFactors.2019;[Epub] CrossRef - Poor Control of Blood Glucose, Lifestyle, and Cardiometabolic Parameters in Younger Adult Patients with Type 2 Diabetes Mellitus
Nam, Han, Joo, Kang, Lim, Kim, Park
Journal of Clinical Medicine.2019; 8(9): 1405. CrossRef - Frailty and Disability in Diabetes
Sol-Ji Yoon, Kwang-il Kim
Annals of Geriatric Medicine and Research.2019; 23(4): 165. CrossRef - A Case Report of Increased Blood Sugar in a Diabetic Patient Treated with Socheongryong-tang
Youngji Kim, Juyeon Song, Seungcheol Hong, Song-won Park, Hakkyeom Kim, Lib Ahn, Dong-jun Choi
The Journal of Internal Korean Medicine.2019; 40(5): 929. CrossRef - A comparison of sotagliflozin therapy for diabetes mellitus between week 24 with week 52
Nie Zhang, Zhi-Qun Gu, Yun-Long Ding, Liu Yang, Mao-Bing Chen, Qi-Han Zheng
Medicine.2019; 98(47): e17976. CrossRef - 2019 Clinical Practice Guidelines for Type 2 Diabetes Mellitus in Korea
Mee Kyoung Kim, Seung-Hyun Ko, Bo-Yeon Kim, Eun Seok Kang, Junghyun Noh, Soo-Kyung Kim, Seok-O Park, Kyu Yeon Hur, Suk Chon, Min Kyong Moon, Nan-Hee Kim, Sang Yong Kim, Sang Youl Rhee, Kang-Woo Lee, Jae Hyeon Kim, Eun-Jung Rhee, SungWan Chun, Sung Hoon Yu
Diabetes & Metabolism Journal.2019; 43(4): 398. CrossRef - Letter: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J2019;43:582–9)
Tae Seo Sohn
Diabetes & Metabolism Journal.2019; 43(6): 909. CrossRef - The Need to Improve the Quality of Diabetes Care in Korea
Seung Jin Han, Dae Jung Kim
Journal of Korean Medical Science.2019;[Epub] CrossRef - Letter: Projection of Diabetes Prevalence in Korean Adults for the Year 2030 Using Risk Factors Identified from National Data (Diabetes Metab J 2019;43:90–6)
Bo Kyung Koo
Diabetes & Metabolism Journal.2019; 43(2): 242. CrossRef - Letter: Efficacy and Safety of Voglibose Plus Metformin in Patients with Type 2 Diabetes Mellitus: A Randomized Controlled Trial (Diabetes Metab J 2019;43;276-86)
Hannah Seok, Tae Seo Sohn
Diabetes & Metabolism Journal.2019; 43(4): 545. CrossRef - Teneligliptin versus sitagliptin in Korean patients with type 2 diabetes inadequately controlled with metformin and glimepiride: A randomized, double‐blind, non‐inferiority trial
Yonghyun Kim, Eun Seok Kang, Hak Chul Jang, Dong Jun Kim, Taekeun Oh, Eun Sook Kim, Nan‐Hee Kim, Kyung Mook Choi, Sung‐Rae Kim, JiYoung You, Se‐Jin Kim, Moon‐Kyu Lee
Diabetes, Obesity and Metabolism.2019; 21(3): 631. CrossRef - Fifty Years of Compassionate Care and Harmonious Collaboration of the Korean Diabetes Association: The 50th Anniversary of Korean Diabetes Association
Jong Chul Won, Eun-Jung Rhee, Hyung Joon Yoo
Diabetes & Metabolism Journal.2018; 42(6): 475. CrossRef
- Impact of anaerobic zone on biodegradation of micropollutants: Comparison of micropollutants’ removal efficiencies in lab-scale anaerobic bioreactor and in full-scale anaerobic zone
- Clinical Care/Education
- Diabetes Camp as Continuing Education for Diabetes Self-Management in Middle-Aged and Elderly People with Type 2 Diabetes Mellitus
- So Young Park, Sun Young Kim, Hye Mi Lee, Kyu Yeon Hur, Jae Hyeon Kim, Moon-Kyu Lee, Kang-Hee Sim, Sang-Man Jin
- Diabetes Metab J. 2017;41(2):99-112. Published online March 3, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.2.99
- 4,172 View
- 43 Download
- 3 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Despite the established benefits of diabetes camps for the continuing education of children with type 1 diabetes mellitus, little is known about the long-term metabolic benefits of diabetes camps for middle-aged and elderly people with type 2 diabetes mellitus (T2DM), especially in terms of glycosylated hemoglobin (HbA1c) variability.
Methods The 1-year mean and variability of HbA1c before and after the diabetes camp was compared between the participants of the diabetes camp (
n =57; median age 65 years [range, 50 to 86 years]; median diabetes duration 14 years [range, 1 to 48 years]). Additional case-control analysis compared the metabolic outcomes of the participants of the diabetes camp and their propensity score-matched controls who underwent conventional diabetes education (n =93).Results The levels of HbA1c during the first year after the diabetes camp were comparable to those of the matched controls (
P =0.341). In an analysis of all participants of the diabetes camp, the 1-year mean±standard deviation (SD) of HbA1c decreased (P =0.010 andP =0.041) after the diabetes camp, whereas the adjusted SD and coefficient of variance (CV) of HbA1c did not decrease. The adjusted SD and CV significantly decreased after the diabetes camp in participants whose 1-year mean HbA1c was ≥6.5% before the diabetes camp (n =40) and those with a duration of diabetes less than 15 years (n =32).Conclusion The 1-year mean and SD of HbA1c decreased after the diabetes camp, with significant reduction in the adjusted SD and CV in those with higher baseline HbA1c and a shorter duration of diabetes.
-
Citations
Citations to this article as recorded by- Older adults’ experiences of being at a senior summer camp—A phenomenographic study
Veronika Wallroth, Kjerstin Larsson, Agneta Schröder
Qualitative Social Work.2022; 21(5): 956. CrossRef - Pushing for miracles, pulling away from risk: An ethnographic analysis of the force dynamics at Senior Summer Camps in Sweden
Gabriella Nilsson, Lisa Ekstam, Janicke Andersson
Journal of Aging Studies.2018; 47: 96. CrossRef
- Older adults’ experiences of being at a senior summer camp—A phenomenographic study
- Others
- Addition of Ipragliflozin to Metformin Treatment in Korean Patients with Type 2 Diabetes Mellitus: Subgroup Analysis of a Phase 3 Trial
- Kyung-Wan Min, Bon Jeong Ku, Ji-Hyun Lee, Min-Seon Kim, Kyu-Jeung Ahn, Moon-Kyu Lee, Satoshi Kokubo, Satoshi Yoshida, Hyun-Ji Cho, Bong-Soo Cha
- Diabetes Metab J. 2017;41(2):135-145. Published online January 11, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.2.135
- 4,943 View
- 59 Download
- 13 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background This is a subgroup analysis of Korean patients from a phase 3 clinical trial investigating the efficacy and safety of ipragliflozin in patients with type 2 diabetes mellitus inadequately controlled with metformin.
Methods This multicenter, placebo-controlled, double-blind, parallel-group study was carried out between November 2011 and January 2013. Patients entered a 2-week placebo pretreatment period, followed by a 24-week treatment period with either ipragliflozin (50 mg/day) or placebo, while continuing metformin. Efficacy outcomes (glycosylated hemoglobin [HbA1c], fasting plasma glucose [FPG], and body weight) and safety outcomes (treatment-emergent adverse events [TEAEs]) were measured and compared between the two treatment groups for patients enrolled in all 18 study sites in Korea.
Results Eighty-two Korean patients received ipragliflozin (
n =43) or placebo (n =39) during the study period. Mean changes in HbA1c levels from baseline to the end of treatment were –0.97% in the ipragliflozin group and –0.31% in the placebo group, with an adjusted between-group difference of –0.60% (P <0.001). Compared to placebo, FPG and body weight also decreased significantly (bothP <0.001) from baseline after treatment in the ipragliflozin group, with between-group differences of –21.4 mg/dL and –1.53 kg, respectively. Decreased weight was the most common TEAE in the ipragliflozin group (7.0%); there were no reports of genital and urinary tract infection.Conclusion Ipragliflozin treatment in addition to metformin led to significant improvement in glycemic outcomes and reduction in body weight in Korean patients with type 2 diabetes mellitus, compared with metformin treatment alone; the safety profile was comparable in both groups.
-
Citations
Citations to this article as recorded by- Add-on therapy with dapagliflozin in routine outpatient care of type 2 diabetes patients from Turkey: a retrospective cohort study on HbA1c, body weight, and blood pressure outcomes
Derun Taner Ertugrul, Erdal Kan, Cigdem Bahadir Tura, Haci Bayram Tugtekin, Hayati Ayakta, Mehmet Celebioglu, Ceren Yılmaz, Onur Utebay, Ilhan Yetkin, Eren Gurkan, Kerem Sezer, Ramazan Gen, Suleyman Ozcaylak, Yildiz Okuturlar, Mehmet Coskun, Nilgun Govec
International Journal of Diabetes in Developing Countries.2022; 42(1): 147. CrossRef SGLT2 Inhibitors as Add-On Therapy to Metformin for People with Type 2 Diabetes: A Review of Placebo-Controlled Trials in Asian versus Non-Asian Patients
André J Scheen
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 2765. CrossRef- Ipragliflozin Additively Ameliorates Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Controlled with Metformin and Pioglitazone: A 24-Week Randomized Controlled Trial
Eugene Han, Yong-ho Lee, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha
Journal of Clinical Medicine.2020; 9(1): 259. CrossRef - Safety of Ipragliflozin in Patients with Type 2 Diabetes Mellitus: Pooled Analysis of Phase II/III/IV Clinical Trials
Atsunori Kashiwagi, Marina V. Shestakova, Yuichiro Ito, Masahiro Noguchi, Wim Wilpshaar, Satoshi Yoshida, John P. H. Wilding
Diabetes Therapy.2019; 10(6): 2201. CrossRef - Mechanistic effects of SGLT2 inhibition on blood pressure in diabetes
Habib Yaribeygi, Stephen L. Atkin, Amirhossein Sahebkar
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(2): 1679. CrossRef - Ipragliflozin as an add-on therapy in type 2 diabetes mellitus patients: An evidence-based pharmacoeconomics evaluation
Hongmei Wang, Gaoqiong Yao, Xi Chen, Jing Ouyang, Jiadan Yang
Diabetes Research and Clinical Practice.2019; 157: 107867. CrossRef - Characteristics of Dapagliflozin Responders: A Longitudinal, Prospective, Nationwide Dapagliflozin Surveillance Study in Korea
Eugene Han, Ari Kim, Sung Jae Lee, Je-Yon Kim, Jae Hyeon Kim, Woo Je Lee, Byung-Wan Lee
Diabetes Therapy.2018; 9(4): 1689. CrossRef - A phase 3 randomized placebo-controlled trial to assess the efficacy and safety of ipragliflozin as an add-on therapy to metformin in Russian patients with inadequately controlled type 2 diabetes mellitus
Marina V. Shestakova, John P.H. Wilding, Wim Wilpshaar, Reiner Tretter, Valeria L. Orlova, Andrey F. Verbovoy
Diabetes Research and Clinical Practice.2018; 146: 240. CrossRef - Efficacy and safety of ipragliflozin as an add‐on therapy to sitagliptin and metformin in Korean patients with inadequately controlled type 2 diabetes mellitus: A randomized controlled trial
Kyung‐Ah Han, Suk Chon, Choon Hee Chung, Soo Lim, Kwan‐Woo Lee, SeiHyun Baik, Chang Hee Jung, Dong‐Sun Kim, Kyong Soo Park, Kun‐Ho Yoon, In‐Kyu Lee, Bong‐Soo Cha, Taishi Sakatani, Sumi Park, Moon‐Kyu Lee
Diabetes, Obesity and Metabolism.2018; 20(10): 2408. CrossRef - Antihyperglycemic Agent Therapy for Adult Patients with Type 2 Diabetes Mellitus 2017: A Position Statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
Diabetes & Metabolism Journal.2017; 41(5): 337. CrossRef - Antihyperglycemic agent therapy for adult patients with type 2 diabetes mellitus 2017: a position statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
The Korean Journal of Internal Medicine.2017; 32(6): 947. CrossRef - Combination therapy of oral hypoglycemic agents in patients with type 2 diabetes mellitus
Min Kyong Moon, Kyu Yeon Hur, Seung-Hyun Ko, Seok-O Park, Byung-Wan Lee, Jin Hwa Kim, Sang Youl Rhee, Hyun Jin Kim, Kyung Mook Choi, Nan-Hee Kim
The Korean Journal of Internal Medicine.2017; 32(6): 974. CrossRef - Combination Therapy of Oral Hypoglycemic Agents in Patients with Type 2 Diabetes Mellitus
Min Kyong Moon, Kyu-Yeon Hur, Seung-Hyun Ko, Seok-O Park, Byung-Wan Lee, Jin Hwa Kim, Sang Youl Rhee, Hyun Jin Kim, Kyung Mook Choi, Nan-Hee Kim
Diabetes & Metabolism Journal.2017; 41(5): 357. CrossRef
- Add-on therapy with dapagliflozin in routine outpatient care of type 2 diabetes patients from Turkey: a retrospective cohort study on HbA1c, body weight, and blood pressure outcomes
- Obesity and Metabolic Syndrome
- Serum Calcium and the Risk of Incident Metabolic Syndrome: A 4.3-Year Retrospective Longitudinal Study
- Jong Ha Baek, Sang-Man Jin, Ji Cheol Bae, Jae Hwan Jee, Tae Yang Yu, Soo Kyoung Kim, Kyu Yeon Hur, Moon-Kyu Lee, Jae Hyeon Kim
- Diabetes Metab J. 2017;41(1):60-68. Published online December 26, 2016
- DOI: https://doi.org/10.4093/dmj.2017.41.1.60
- 4,066 View
- 32 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background An association between serum calcium level and risk of metabolic syndrome (MetS) has been suggested in cross-sectional studies. This study aimed to evaluate the association between baseline serum calcium level and risk of incident MetS in a longitudinal study.
Methods We conducted a retrospective longitudinal study of 12,706 participants without MetS who participated in a health screening program, had normal range serum calcium level at baseline (mean age, 51 years), and were followed up for 4.3 years (18,925 person-years). The risk of developing MetS was analyzed according to the baseline serum calcium levels.
Results A total of 3,448 incident cases (27.1%) of MetS developed during the follow-up period. The hazard ratio (HR) for incident MetS did not increase with increasing tertile of serum calcium level in an age- and sex-matched model (
P for trend=0.915). The HRs (95% confidence interval [CI]) for incident MetS comparing the second and the third tertiles to the first tertile of baseline serum calcium level were 0.91 (95% CI, 0.84 to 0.99) and 0.85 (95% CI, 0.78 to 0.92) in a fully adjusted model, respectively (P for trend=0.001). A decreased risk of incident MetS in higher tertiles of serum calcium level was observed in subjects with central obesity and/or a metabolically unhealthy state at baseline.Conclusion There was no positive correlation between baseline serum calcium levels and incident risk of MetS in this longitudinal study. There was an association between higher serum calcium levels and decreased incident MetS in individuals with central obesity or two components of MetS at baseline.
-
Citations
Citations to this article as recorded by- Independent associations of serum calcium with or without albumin adjustment and serum phosphorus with nonalcoholic fatty liver disease: results from NHANES 1999-2018
Haolong Qi, Bin Wang, Lei Zhu
Frontiers in Endocrinology.2024;[Epub] CrossRef - Association of the serum calcium level with metabolic syndrome and its components among adults in Taiwan
Jer-min Chen, Tai-yin Wu, Yi-fan Wu, Kuan-liang Kuo
Archives of Endocrinology and Metabolism.2023;[Epub] CrossRef - Elevated Chinese visceral adiposity index increases the risk of stroke in Chinese patients with metabolic syndrome
Zeyu Liu, Qin Huang, Bi Deng, Minping Wei, Xianjing Feng, Fang Yu, Jie Feng, Yang Du, Jian Xia
Frontiers in Endocrinology.2023;[Epub] CrossRef - Metformin: Expanding the Scope of Application—Starting Earlier than Yesterday, Canceling Later
Yulia A. Kononova, Nikolai P. Likhonosov, Alina Yu. Babenko
International Journal of Molecular Sciences.2022; 23(4): 2363. CrossRef - Metformin in prediabetes: key mechanisms for the prevention of diabetes and cardiometabolic risks
A. Yu. Babenko
Meditsinskiy sovet = Medical Council.2022; (10): 96. CrossRef Calcium and Phosphate Levels are Among Other Factors Associated with Metabolic Syndrome in Patients with Normal Weight
Kamila Osadnik, Tadeusz Osadnik, Marcin Delijewski, Mateusz Lejawa, Martyna Fronczek, Rafał Reguła, Mariusz Gąsior, Natalia Pawlas
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 1281. CrossRef- Association between selected trace elements and body mass index and waist circumference: A cross sectional study
Mahnaz Zohal, Saeedeh Jam-Ashkezari, Nasim Namiranian, Amin Moosavi, Akram Ghadiri-Anari
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(2): 1293. CrossRef - Letter: Increased Serum Angiopoietin-Like 6 Ahead of Metabolic Syndrome in a Prospective Cohort Study (Diabetes Metab J 2019;43:521-9)
Jin Hwa Kim
Diabetes & Metabolism Journal.2019; 43(5): 727. CrossRef - Genotype effects of glucokinase regulator on lipid profiles and glycemic status are modified by circulating calcium levels: results from the Korean Genome and Epidemiology Study
Oh Yoen Kim, So-Young Kwak, Hyunjung Lim, Min-Jeong Shin
Nutrition Research.2018; 60: 96. CrossRef
- Independent associations of serum calcium with or without albumin adjustment and serum phosphorus with nonalcoholic fatty liver disease: results from NHANES 1999-2018
- Effectiveness of 3-Day Continuous Glucose Monitoring for Improving Glucose Control in Type 2 Diabetic Patients in Clinical Practice
- Soo Kyoung Kim, Hye Jeong Kim, Taehun Kim, Kyu Yeon Hur, Sun Wook Kim, Moon-Kyu Lee, Yong-Ki Min, Kwang-Won Kim, Jae Hoon Chung, Jae Hyeon Kim
- Diabetes Metab J. 2014;38(6):449-455. Published online December 15, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.6.449
- 4,861 View
- 38 Download
- 16 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aim of this study was to investigate whether adjusting diabetic treatment regimens according to the information obtained from a continuous glucose monitoring system (CGMS) might lead to improved glycemic control in patients with type 2 diabetes.
Methods We reviewed the medical charts of 172 patients who used the CGMS for 1 year starting in December 2008 and the records of 1,500 patients who visited their regular outpatient clinics during December 2008. Of these patients, a total of 65 CGMS patients and 301 regular outpatients (control group) were enrolled in the study after propensity score matching. There were no differences in baseline glycated hemoglobin (HbA1c), age, and duration of diabetes between the CGMS and the control groups after propensity score matching. The changes in the HbA1c levels from baseline to 6 months were calculated.
Results The CGMS group showed a significant improvement in the HbA1c level compared to the control group at 3 months (7.9%±1.6% vs. 7.4%±1.2%,
P =0.001) and at 6 months (7.4%±1.2% vs. 7.9%±1.6%,P =0.010). There were significant differences in the treatment modality changes between the CGMS group and the control group.Conclusion Using a 3-day CGMS was advantageous for improving glucose control in patients with type 2 diabetes and may help these patients to optimize glycemic control in clinical practice.
-
Citations
Citations to this article as recorded by- Biological and Clinical Impacts of Glucose Metabolism in Pancreatic Ductal Adenocarcinoma
Zhao Liu, Hiromitsu Hayashi, Kazuki Matsumura, Norio Uemura, Yuta Shiraishi, Hiroki Sato, Hideo Baba
Cancers.2023; 15(2): 498. CrossRef - Professional continuous glucose monitoring in patients with diabetes mellitus: A systematic review and meta‐analysis
Sergio Di Molfetta, Irene Caruso, Angelo Cignarelli, Annalisa Natalicchio, Sebastio Perrini, Luigi Laviola, Francesco Giorgino
Diabetes, Obesity and Metabolism.2023; 25(5): 1301. CrossRef - American Association of Clinical Endocrinology Clinical Practice Guideline: The Use of Advanced Technology in the Management of Persons With Diabetes Mellitus
George Grunberger, Jennifer Sherr, Myriam Allende, Thomas Blevins, Bruce Bode, Yehuda Handelsman, Richard Hellman, Rosemarie Lajara, Victor Lawrence Roberts, David Rodbard, Carla Stec, Jeff Unger
Endocrine Practice.2021; 27(6): 505. CrossRef - Lack of Acceptance of Digital Healthcare in the Medical Market: Addressing Old Problems Raised by Various Clinical Professionals and Developing Possible Solutions
Jong Il Park, Hwa Young Lee, Hyunah Kim, Jisan Lee, Jiwon Shinn, Hun-Sung Kim
Journal of Korean Medical Science.2021;[Epub] CrossRef - A head‐to‐head comparison of personal and professional continuous glucose monitoring systems in people with type 1 diabetes: Hypoglycaemia remains the weak spot
Othmar Moser, Marlene Pandis, Felix Aberer, Harald Kojzar, Daniel Hochfellner, Hesham Elsayed, Melanie Motschnig, Thomas Augustin, Philipp Kreuzer, Thomas R. Pieber, Harald Sourij, Julia K. Mader
Diabetes, Obesity and Metabolism.2019; 21(4): 1043. CrossRef - Glucose monitoring in diabetes: from clinical studies to real‐world practice
Rebecca C Sagar, Afroze Abbas, Ramzi Ajjan
Practical Diabetes.2019; 36(2): 57. CrossRef - The Effectiveness of Continuous Glucose Monitoring in Patients with Type 2 Diabetes: A Systematic Review of Literature and Meta-analysis
Cindy Park, Quang A. Le
Diabetes Technology & Therapeutics.2018; 20(9): 613. CrossRef - Effects of Dapagliflozin on 24-Hour Glycemic Control in Patients with Type 2 Diabetes: A Randomized Controlled Trial
Robert R. Henry, Poul Strange, Rong Zhou, Jeremy Pettus, Leon Shi, Sergey B. Zhuplatov, Traci Mansfield, David Klein, Arie Katz
Diabetes Technology & Therapeutics.2018; 20(11): 715. CrossRef - Clinical and economic benefits of professional CGM among people with type 2 diabetes in the United States: analysis of claims and lab data
Joseph A. Sierra, Mona Shah, Max S. Gill, Zachery Flores, Hiten Chawla, Francine R. Kaufman, Robert Vigersky
Journal of Medical Economics.2018; 21(3): 225. CrossRef - Role of continuous glucose monitoring for type 2 in diabetes management and research
Robert Vigersky, Maneesh Shrivastav
Journal of Diabetes and its Complications.2017; 31(1): 280. CrossRef - Assessing the Therapeutic Utility of Professional Continuous Glucose Monitoring in Type 2 Diabetes Across Various Therapies: A Retrospective Evaluation
Jothydev Kesavadev, Robert Vigersky, John Shin, Pradeep Babu Sadasivan Pillai, Arun Shankar, Geethu Sanal, Gopika Krishnan, Sunitha Jothydev
Advances in Therapy.2017; 34(8): 1918. CrossRef - Use of Continuous Glucose Monitoring in Youth-Onset Type 2 Diabetes
Christine L. Chan
Current Diabetes Reports.2017;[Epub] CrossRef - The efficacy and safety of adding either vildagliptin or glimepiride to ongoing metformin therapy in patients with type 2 diabetes mellitus
Gyuri Kim, Sewon Oh, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim, Moon-Kyu Lee
Expert Opinion on Pharmacotherapy.2017; 18(12): 1179. CrossRef - Morning Spot Urine Glucose-to-Creatinine Ratios Predict Overnight Urinary Glucose Excretion in Patients With Type 2 Diabetes
So Ra Kim, Yong-ho Lee, Sang-Guk Lee, Sun Hee Lee, Eun Seok Kang, Bong-Soo Cha, Hyun Chul Lee, Jeong-Ho Kim, Byung-Wan Lee
Annals of Laboratory Medicine.2017; 37(1): 9. CrossRef - The Contemporary Role of Masked Continuous Glucose Monitoring in a Real-Time World
Ian Blumer
Journal of Diabetes Science and Technology.2016; 10(3): 790. CrossRef - Glycemic Variability: How Do We Measure It and Why Is It Important?
Sunghwan Suh, Jae Hyeon Kim
Diabetes & Metabolism Journal.2015; 39(4): 273. CrossRef
- Biological and Clinical Impacts of Glucose Metabolism in Pancreatic Ductal Adenocarcinoma
- Smaller Mean LDL Particle Size and Higher Proportion of Small Dense LDL in Korean Type 2 Diabetic Patients
- Sunghwan Suh, Hyung-Doo Park, Se Won Kim, Ji Cheol Bae, Alice Hyun-Kyung Tan, Hye Soo Chung, Kyu Yeon Hur, Jae Hyeon Kim, Kwang-Won Kim, Moon-Kyu Lee
- Diabetes Metab J. 2011;35(5):536-542. Published online October 31, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.5.536
- 4,623 View
- 39 Download
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Small dense low density lipoprotein (sdLDL) has recently emerged as an important risk factor of coronary heart disease.
Methods The mean LDL particle size was measured in 203 patients with type 2 diabetes mellitus (T2DM) and 212 matched subjects without diabetes using polyacrylamide tube gel electrophoresis. Major vascular complications were defined as stroke, angiographically-documented coronary artery disease or a myocardial infarction. Peripheral vascular stenosis, carotid artery stenosis (≥50% in diameter) or carotid artery plaque were considered minor vascular complications. Overall vascular complications included both major and minor vascular complications.
Results Diabetic patients had significantly smaller mean-LDL particle size (26.32 nm vs. 26.49 nm) and a higher percentage of sdLDL to total LDL compared to those of subjects without diabetes (21.39% vs. 6.34%). The independent predictors of sdLDL in this study were serum triglyceride level and body mass index (odds ratio [OR], 1.020 with
P <0.001 and OR 1.152 withP <0.027, respectively). However, no significant correlations were found between sdLDL and major vascular complications (P =0.342), minor vascular complications (P =0.573) or overall vascular complications (P =0.262) in diabetic subjects.Conclusion Diabetic patients had a smaller mean-LDL particle size and higher proportion of sdLDL compared to those of subjects without diabetes. Obese diabetic patients with hypertriglyceridemia have an increased risk for atherogenic small dense LDL. However, we could not verify an association between LDL particle size and vascular complications in this study.
-
Citations
Citations to this article as recorded by- Evaluation of measured and calculated small dense low-density lipoprotein in capillary blood and association with the metabolic syndrome
Sara Deza, Inmaculada Colina, Oscar Beloqui, José Ignacio Monreal, Estéfani Martínez-Chávez, Julia Maroto-García, Carmen Mugueta, Alvaro González, Nerea Varo
Clinica Chimica Acta.2024; 557: 117897. CrossRef - Association between measured or calculated small dense low‐density lipoprotein cholesterol and oxidized low‐density lipoprotein in subjects with or without type 2 diabetes mellitus
Hyun‐Ki Kim, Jinyoung Hong, Sunyoung Ahn, Woochang Lee, Sail Chun, Won‐Ki Min
Journal of Clinical Laboratory Analysis.2023;[Epub] CrossRef - The association of apolipoprotein in the risk of ST-elevation myocardial infarction in patients with documented coronary artery disease
Astuti Giantini, Nur Gifarani Pratiwi, Renan Sukmawan, Joedo Prihartono, Suzanna Immanuel, Merci Monica Pasaribu, Sri Suryo Adiyanti, Yusuf Bahasoan
International Journal of Cardiology Cardiovascular Risk and Prevention.2023; 18: 200194. CrossRef - Atherogenic Index of Plasma and Its Association with Risk Factors of Coronary Artery Disease and Nutrient Intake in Korean Adult Men: The 2013–2014 KNHANES
Hye Ran Shin, SuJin Song, Jin Ah Cho, Sun Yung Ly
Nutrients.2022; 14(5): 1071. CrossRef - The Atherogenic Index of Plasma: A Powerful and Reliable Predictor for Coronary Artery Disease in Patients With Type 2 Diabetes
Kuo Zhou, Zheng Qin, Jinfan Tian, Kongyong Cui, Yunfeng Yan, Shuzheng Lyu
Angiology.2021; 72(10): 934. CrossRef - Direct bilirubin is associated with low-density lipoprotein subfractions and particle size in overweight and centrally obese women
Y.-J. Kwon, H.-S. Lee, J.-W. Lee
Nutrition, Metabolism and Cardiovascular Diseases.2018; 28(10): 1021. CrossRef - Correlation between Cholesterol, Triglycerides, Calculated, and Measured Lipoproteins: Whether Calculated Small Density Lipoprotein Fraction Predicts Cardiovascular Risks
Sikandar Hayat Khan, Nadeem Fazal, Athar Abbas Gilani Shah, Syed Mohsin Manzoor, Naveed Asif, Aamir Ijaz, Najmusaqib Khan Niazi, Muhammad Yasir
Journal of Lipids.2017; 2017: 1. CrossRef - Effects of Small Dense LDL in Diabetic Nephropathy in Females with Type 2 Diabetes Mellitus
Seongyul Ryu, Youngwoo Kim, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Hyun Baek, Ki-Ho Song, Kyung-Jin Yun
Journal of Lipid and Atherosclerosis.2016; 5(1): 11. CrossRef - Prepregnancy Adverse Lipid Profile and Subsequent Risk of Gestational Diabetes
Emily S. Han, Ronald M. Krauss, Fei Xu, Sneha B. Sridhar, Assiamira Ferrara, Charles P. Quesenberry, Monique M. Hedderson
The Journal of Clinical Endocrinology & Metabolism.2016; 101(7): 2721. CrossRef - Meta-analysis of Atherogenic Index of Plasma and other lipid parameters in relation to risk of type 2 diabetes mellitus
Xiao-Wei Zhu, Fei-Yan Deng, Shu-Feng Lei
Primary Care Diabetes.2015; 9(1): 60. CrossRef - Higher levels of small dense low‐density lipoprotein (LDL) are associated with cardiac autonomic neuropathy in patients with Type 2 diabetes
E.‐H. Jang, Y.‐M. Park, J. Hur, M.‐K. Kim, S.‐H. Ko, K.‐H. Baek, K.‐H. Song, K.‐W. Lee, H.‐S. Kwon
Diabetic Medicine.2013; 30(6): 694. CrossRef - Sleep Status and Low-Density Lipoprotein Particle Size in a General Japanese Female Population: The Mima Study
Kazuhiko Kotani, Kokoro Tsuzaki, Shinji Fujiwara, Naoki Sakane
Medical Principles and Practice.2013; 22(5): 510. CrossRef - Serum small-dense LDL abnormalities in chronic renal disease patients
M. Chu, A. Y. M. Wang, I. H. S. Chan, S. H. Chui, C. W. K. Lam
British Journal of Biomedical Science.2012; 69(3): 99. CrossRef - Small Dense Low-density Lipoprotein and Cardiovascular Disease
Sunghwan Suh, Moon-Kyu Lee
Journal of Lipid and Atherosclerosis.2012; 1(1): 1. CrossRef
- Evaluation of measured and calculated small dense low-density lipoprotein in capillary blood and association with the metabolic syndrome
- Efficacy of Sitagliptin When Added to Ongoing Therapy in Korean Subjects with Type 2 Diabetes Mellitus
- Hye Soo Chung, Moon-Kyu Lee
- Diabetes Metab J. 2011;35(4):411-417. Published online August 31, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.4.411
- 3,402 View
- 73 Download
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background To evaluate the clinical efficacy of sitagliptin for reducing plasma glucose levels in Korean subjects with type 2 diabetes mellitus during a 14-week treatment period.
Methods Our study design involved the addition of 100 mg sitagliptin once-daily to three ongoing combination therapy regimens and changing from glimepiride and metformin to sitagliptin and metformin.
Results The addition of sitagliptin 100 mg/day produced a statistically significant reduction in mean HbA1c level (mean HbA1c reduction of 0.99±0.85%,
P <0.01). In the group taking a combination of sitagliptin and metformin (n =143, initial mean HbA1c level=7.48%), the reductions in HbA1c, 2-hour postprandial glucose, and fasting glucose levels were 0.72±0.76% (P <0.01), 47±65 mg/dL (P <0.01), and 15±44 mg/dL (P <0.01), respectively. In the group taking a combination of sitagliptin, glimepiride, and metformin (n =125, initial mean HbA1c level=8.42%), the reductions in HbA1c, 2-hour postprandial glucose, and fasting glucose levels were 1.09±0.86% (P <0.01), 62±64 mg/dL (P <0.01), and 31±45 mg/dL (P <0.01), respectively. In the group taking a combination of sitagliptin, glimepiride, metformin, and α-glucosidase inhibitor (n =63, initial mean HbA1c level=9.19%), the reductions in HbA1c, 2-hour postprandial glucose, and fasting glucose levels were 1.27±0.70% (P <0.01), 72±65 mg/dL (P <0.01), and 35±51 mg/dL (P <0.01), respectively. In the group that had previous hypoglycemic events and that changed from glimepiride to sitagliptin, HbA1c level did not change but fasting glucose increased significantly (14±29 mg/dL,P <0.01).Conclusion Sitagliptin combination therapy for 14 weeks significantly improved glycemic control and was well-tolerated in Korean subjects with type 2 diabetes mellitus.
-
Citations
Citations to this article as recorded by- Impact of Treviamet® & Treviamet XR® on quality of life besides glycemic control in type 2 DM patients
Asima Khan, Muhammad Adnan Kanpurwala, Riasat Ali Khan, Najum F. Mahmudi, Verumal Lohano, Shakeel Ahmed, Majid Khan, Fareed Uddin, Syed Mohammad Ali, Maliha Saghir, Syed Hussain Baqar Abidi, Jahanzeb Kamal
BMC Endocrine Disorders.2023;[Epub] CrossRef - Efficacy and safety of sitagliptin/metformin fixed‐dose combination compared with glimepiride in patients with type 2 diabetes: A multicenter randomized double‐blind study
Sang Soo Kim, In Joo Kim, Kwang Jae Lee, Jeong Hyun Park, Young Il Kim, Young Sil Lee, Sung Chang Chung, Sang Jin Lee
Journal of Diabetes.2017; 9(4): 412. CrossRef - Optimal Candidates for the Switch from Glimepiride to Sitagliptin to Reduce Hypoglycemia in Patients with Type 2 Diabetes Mellitus
Hyun Min Kim, Jung Soo Lim, Byung-Wan Lee, Eun-Seok Kang, Hyun Chul Lee, Bong-Soo Cha
Endocrinology and Metabolism.2015; 30(1): 84. CrossRef - Effectiveness and safety of glimepiride and iDPP4, associated with metformin in second line pharmacotherapy of type 2 diabetes mellitus: systematic review and meta‐analysis
JM. Amate, T. Lopez‐Cuadrado, N. Almendro, C. Bouza, Z. Saz‐Parkinson, R. Rivas‐Ruiz, J. Gonzalez‐Canudas
International Journal of Clinical Practice.2015; 69(3): 292. CrossRef - Clinical Characteristics and Metabolic Predictors of Rapid Responders to Dipeptidyl Peptidase-4 Inhibitor as an Add-on Therapy to Sulfonylurea and Metformin
Ye An Kim, Won Sang Yoo, Eun Shil Hong, Eu Jeong Ku, Kyeong Seon Park, Soo Lim, Young Min Cho, Kyong Soo Park, Hak Chul Jang, Sung Hee Choi
Diabetes & Metabolism Journal.2015; 39(6): 489. CrossRef - Sitagliptin for Elderly Patients Aged 75 Years or Older with Inadequately Controlled Type 2 Diabetes with Common Antidiabetes Treatments
Katsunori Suzuki, Yurie Mistuma, Takaaki Sato, Mariko Hatta
International Journal of Clinical Medicine.2015; 06(09): 672. CrossRef - Short‐ and long‐term effect of sitagliptin after near normalization of glycemic control with insulin in poorly controlled Japanese type 2 diabetic patients
Keiko Fujisawa, Tetsuyuki Yasuda, Hideaki Kaneto, Naoto Katakami, Mayumi Tsuji, Fumiyo Kubo, Shugo Sasaki, Kazuyuki Miyashita, Toyoko Naka, Ryuuichi Kasami, Akio Kuroda, Munehide Matsuhisa, Iichiro Shimomura
Journal of Diabetes Investigation.2014; 5(5): 548. CrossRef - Efficacy and safety of vildagliptin, Saxagliptin or Sitagliptin as add-on therapy in Chinese patients with type 2 diabetes inadequately controlled with dual combination of traditional oral hypoglycemic agents
Chun-Jun Li, Xiao-Juan Liu, Lian Bai, Qian Yu, Qiu-Mei Zhang, Pei Yu, De-Min Yu
Diabetology & Metabolic Syndrome.2014;[Epub] CrossRef - Tolerability, effectiveness and predictive parameters for the therapeutic usefulness of exenatide in obese, Korean patients with type 2 diabetes
Sun Ok Song, Kwang Joon Kim, Byung‐Wan Lee, Eun Seok Kang, Bong Soo Cha, Hyun Chul Lee
Journal of Diabetes Investigation.2014; 5(5): 554. CrossRef - Efficacy of vildagliptin on glucose fluctuation in Japanese type 2 diabetic patients with ongoing sulfonylurea based oral glycemic agent therapy
Keiji Yoshioka, Haruhiko Isotani, Shin-ichiro Ohashi, Minoru Imamura
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2013; 7(1): 32. CrossRef - Glimepiride Strongly Enhances the Glucose-Lowering Effect in Triple Oral Antidiabetes Therapy with Sitagliptin and Metformin for Japanese Patients with Type 2 Diabetes Mellitus
Keiko Arai, Hajime Maeda, Sin-ichiro Sirabe, Ritsuko Yamamoto, Mikio Yamauchi, Tetsuyuki Hirao, Setsuko Hirao, Koichi Hirao
Diabetes Technology & Therapeutics.2013; 15(4): 335. CrossRef - Efficacy of sitagliptin on blood glucose fluctuation in Japanese type 2 diabetic patients with basal-supported oral therapy
Mitsuyoshi Takahara, Toshihiko Shiraiwa, Hideaki Kaneto, Naoto Katakami, Taka-aki Matsuoka, Iichiro Shimomura
Endocrine Journal.2012; 59(12): 1131. CrossRef
- Impact of Treviamet® & Treviamet XR® on quality of life besides glycemic control in type 2 DM patients

 KDA
KDA
 First
First Prev
Prev





